MR defecography (MRD) now plays a central role in the preoperative evaluation of patients with pelvic floor dysfunction, award-winning researchers have reported.
“MRD can identify surgically relevant findings that are not apparent on physical examination,” noted Dr. Nitin Venugopal and colleagues from the department of radiology at the University of Washington, who won a magna cum laude award for their ECR 2025 e-poster. “MRD is especially useful for assessing the posterior compartment to identify patients who need multidisciplinary surgical management.”
Obstructive defecation or defecatory dysfunction not explained by physical exam should always be evaluated with MRD, particularly in cases of peritoneocele, enterocele, sigmoidocele, and rectal prolapse. Also, defecatory effort should be documented in reports because evaluation is highly dependent on patient effort and cooperation, they added.
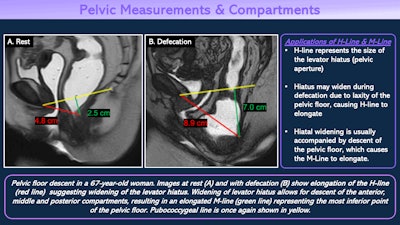 Applications of the H-line and M-line. All figures courtesy of Dr. Nitin Venugopal et al, Department of Radiology, University of Washington, and presented at ECR 2025.
Applications of the H-line and M-line. All figures courtesy of Dr. Nitin Venugopal et al, Department of Radiology, University of Washington, and presented at ECR 2025.
Pelvic organ prolapse affects 40% to 60% of women who have given birth to one or more babies and is frequently multicompartmental. “Involved compartments dictate surgical management and prognosis. Rectal prolapse is often concurrent with advanced pelvic organ prolapse and often requires combined management by both urogynecology and colorectal surgery specialists,” the authors pointed out.
Concurrent anterior and middle compartment prolapse is seen in up to 21% to 34% of patients with rectal prolapse, and operative success ranges from 19% to 97%. Combined repair of pelvic organ prolapse and rectal prolapse is associated with better outcomes, they explained.
Interpretation of MR defecography requires knowledge of the relevant anatomic compartments and their contents: anterior compartment (bladder, urethra), middle compartment (vagina, uterus), and posterior compartment (rectum).
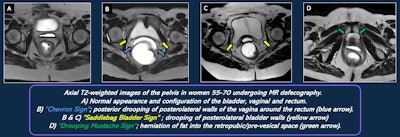 Signs of endopelvic fascial defects on MR defecography.
Signs of endopelvic fascial defects on MR defecography.
Anatomic relationships within the compartments can be described further with the pubococcygeal line (inferior pubic symphysis to the most inferior coccygeal joint plane of levator muscle/pelvic floor), H-line (symphysis to posterior anorectal junction, anteroposterior diameter of levator hiatus, < 6 cm normal), and M-line (perpendicular to pubococcygeal line and intersects posterior H-line, reference for descent of hiatus, < 2 cm considered normal).
“MR defecography is a dynamic exam, with images acquired during multiple phases of straining and defecation. It provides a greater level of anatomic detail and direct visualization of structures, but, unlike fluoroscopy, it is performed in a nonanatomic position,” the Washington team noted.
Individual components of the fascia are often not well visualized with a standard MRD technique, and defects are often inferred indirectly due to secondary findings. An endovaginal coil may improve visualization.
The term “anterior vaginal wall prolapse” is preferred by surgeons because it correlates with the physical exam findings of anterior vaginal wall bulge, the authors stated. The bladder neck descends below the pubococcygeal line. This condition is managed by urogynecology or female urology service.
MRD is important in the detection of a peritoneocele that cannot be reliably detected with clinical exam, and a peritoneocele should prompt the search for an enterocele or a sigmoidocele. Reevaluate the peritoneocele on all defecation attempts to look for the bowel, and isolated defects can be repaired via a transvaginal or transanal approach, they continued. A sigmoidocele may require concomitant sigmoidopexy or sigmoidectomy.
Terminology and reporting
The Pelvic Floor Disorders Consortium (PFDC) provides a consensus definition and interpretation template. MRD can be performed either upright or sitting. Rectal contrast is essential for these exams, and vaginal contrast medium is not routinely required.
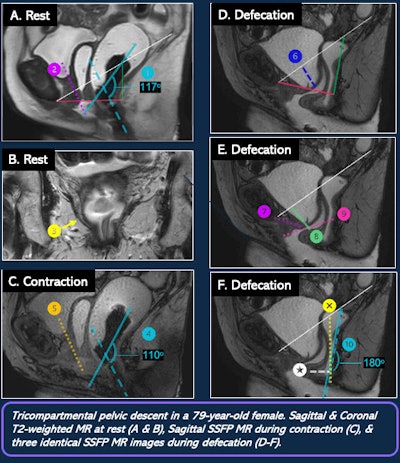 MR defecography exam on a 79-year-old woman.
MR defecography exam on a 79-year-old woman.
Overall, a physical exam is considered reliable for evaluations of the anterior and middle compartments, and anterior and posterior vaginal wall prolapse and apical prolapse are palpable on examination. A Q-tip test is recommended for urethral hypermobility.
MRD provides most value in evaluation of the posterior compartment, and it may reveal pathology not detected by physical exam and requiring concurrent intervention from a nongynecologic surgeon (e.g., colorectal). The most common reasons to evaluate a patient with MRD are obstructive defecation not explained by physical exam and defecatory dysfunction not explained by physical exam, according to Venugopal, who is a radiology resident, and colleagues.
Involved compartments dictate the choice of primary surgical service. Anterior and middle compartment disorders are usually handled by urogynecology or female urology, while most posterior compartment disorders necessitate colorectal surgery. Surgical treatment strategies are divided into reconstructive and obliterative approaches, obliterative procedures close off a portion of the vaginal canal to correct prolapse in patients who no longer require vaginal function (no desire for future sexual activity), the authors concluded.
You can see more clinical cases and figures and read the full ECR 2025 poster here. The co-authors of this exhibit were Drs. Bahar Mansoori and Puneet Bhargava.