By accounting for the presence of the magnetic field during treatment planning, it is possible to deliver clinically acceptable MR-guided lung stereotactic body radiotherapy treatments, report U.K. researchers. Allaying concerns over potential dose distortions, this result may pave the way toward improved radiotherapy treatments.
During radiotherapy, lung tumors can undergo both deformations and movements of up to a few centimeters. If not accounted for, these shifts can lead to underdosage of the target tumor and unwanted extra irradiation of the surrounding tissues. Given this, the integration of MRI with radiation treatments is an attractive prospect: allowing for the real-time acquisition of images, with excellent soft-tissue contrast, during patient treatment. When combined with multileaf collimator tumor tracking, such images can be used to dynamically reoptimize treatment plans to account for observed changes in patient anatomy.
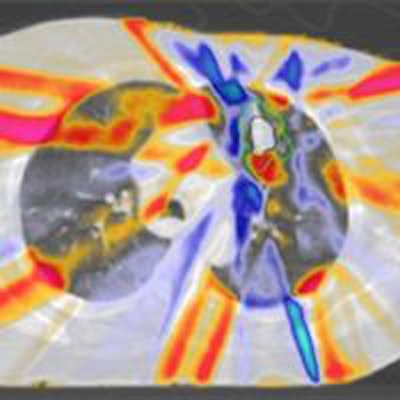
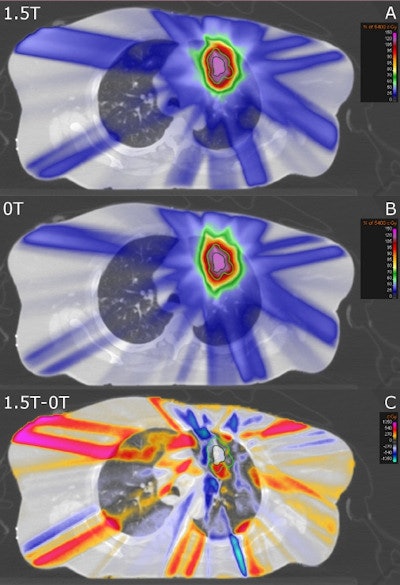 Transversal CT slice of a lung cancer patient overlaid with the simulated dose accumulated on the reference 4D CT phase with a 1.5-tesla magnetic field present (A), the delivered dose without a magnetic field (B) and the difference between those two distributions (C). The GTV is contoured in dark green and the ITV + 5 mm is contoured in light green. Credit: Menten et al/Elsevier.
Transversal CT slice of a lung cancer patient overlaid with the simulated dose accumulated on the reference 4D CT phase with a 1.5-tesla magnetic field present (A), the delivered dose without a magnetic field (B) and the difference between those two distributions (C). The GTV is contoured in dark green and the ITV + 5 mm is contoured in light green. Credit: Menten et al/Elsevier.Despite the potential benefits of this approach, however, concerns have been raised that radiotherapy doses delivered during MR scanning might become distorted. Within the scanner's magnetic field, the Lorentz force could alter the path of the secondary electrons responsible for the absorbed dose, causing them to travel along spiral trajectories, rather than in straight lines.
The treatment of lung tumors may be particularly affected by this, as the distorting phenomena would be pronounced at air-tissue interfaces, explained paper author Martin Menten, a medical physicist at the Institute of Cancer Research in London (Radiotherapy Oncology, June 2016, Vol. 119:3, pp. 461-466).
"When entering low-density material, such as lung tissue or air, the range of travel of these electrons often increases sufficiently such that they can return to their surface of entrance," he noted. "This so-called electron return effect causes local dose 'hot spots' at air-tissue interfaces."
A variety of strategies have been proposed to address these perturbations -- such as using altered magnetic-field and photon-beam geometries, limiting the strength of the magnetic field, or accounting for the distorting during treatment plan optimization. Exploring the latter solution in their new study, Menten and colleagues simulated lung stereotactic body radiotherapy with an MR-linac, for nine patients. For each patient, simulations were run both with and without real-time multileaf collimator tumor tracking, as well as within a 1.5-tesla magnetic field and without.
When radiotherapy treatment was undertaken in the magnetic field, the researchers observed slight dose distortions at air-tissue interface -- resulting, for example, in a 1.4 Gy average increase in dosage to 2% of the skin.
At the same time, the team found the magnetic field did not limit the ability of multileaf collimator tumor tracking to decrease the dose exposure of healthy tissues while still maintaining the target dose to the tumor.
Bryan Bednarz, a medical physicist at the University of Wisconsin-Madison who was not involved in this study, comments that the clinical adoption of disruptive technologies like MR-guided radiotherapy is far from trivial. "In the case of MR-linacs, magnetic fields introduce new challenges during treatment planning, which need to be investigated to ensure the patient is treated in the safest possible manner," he said.
"While the proof of the pudding is in the eating, this work helps convince us that some of these challenges are manageable and clinical gains from this technology are plausible."
"It's exciting to see work progressing on real-time MR-guided radiation therapy," added Charles Kirkby, a medical physicist at the University of Calgary who was also not involved in this study. "Coupled with the image quality available through MRI, there is tremendous potential for this technology to improve the quality of stereotactic body radiotherapy treatments for the treatment of lung tumors."
With this study complete, the researchers are continuing to work on implementing real-time adaptive radiotherapy on a MR-linac platform. "We anticipate that we can adapt our in-house multileaf collimator tracking control software for the MR-linac at our institution in 2017," Menten told medicalphysicsweb, adding that his team is presently developing specialized MR-sequences and image processing techniques to enable localization of tumor and healthy tissues during dose deliveries.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.