Reduced coronary blood flow can predict future cardiovascular events in patients with suspected stable coronary artery disease (CAD), according to research presented on 11 December at the European Association of Cardiovascular Imaging (EACVI) annual congress in Vienna.
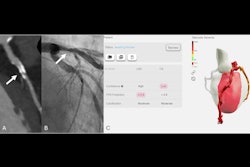
In a study involving 7,836 patients who underwent coronary CT angiography (CCTA), researchers used an AI tool to measure CT-derived fractional flow reserve (FFR-CT), with lower values associated with higher cardiovascular event rates.
“We already know that FFR-CT is valuable for the diagnosis of stable CAD, but whether FFR-CT could also be used prognostically, to predict future major cardiovascular events, is not fully understood,” noted Dr. Jack Bell, of the Liverpool Heart and Chest Hospital, U.K., and colleagues, in a news release from EACVI.
Among the 7,836 patients, the median age was 63, and 37.4% were female. At a median follow-up of 3.1 years, 191 (2.4%) experienced myocardial infarction (MI), 1,573 (20.1%) underwent coronary artery bypass grafting or stenting (revascularizations), 74 (0.9%) died from cardiovascular-specific causes, and 261 (3.3%) had all-cause deaths.
According to the analysis, FFR-CT categories incrementally stratified risk of MI (p < 0.001), revascularization (p < 0.001), cardiovascular mortality (p < 0.001), and all-cause mortality (p = 0.002) over time. For example, MI occurred in 1% of patients with normal FFR-CT, 2% of patients with borderline FFR-CT, 3.9% of those with reduced FFR-CT, and in 5.2% of those with severely reduced FFR-CT, Bell noted.
“This study is the first to provide conclusive evidence of FFR-CT’s prognostic power, independent of other risk factors. We observed that even so-called ‘borderline’ FFR-CT was associated with worse outcomes compared with normal values,” added senior author Dr. Timothy Fairbairn, a consultant cardiologist at the Liverpool Heart and Chest Hospital.
Ultimately, FFR-CT could be used to inform personalized risk assessment, allowing clinicians to provide more intensive, bespoke treatment to those at high risk, the researchers concluded.