A deep-learning model for assessing vessel-specific coronary ischemia has performed well compared with fractional flow reserve (FFR) in a new Belgian study published on 11 October in European Radiology.
The research group, led by radiologist Dr. Benjamin Peters of Hasselt University in Diepenbeek, evaluated a new CT angiography-based FFR (CT-FFRAI) model (CorEx, SPIMED-AI) using images from patients at two centers who underwent coronary CT angiography (CCTA) and invasive FFR and/or instantaneous wave-free ratio (iFR) measurements.
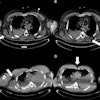
 False-positive case. A representative case of an 81-year-old male patient with a recent onset of stable chest pain. Curved multiplanar reconstruction coronary computed tomography angiography (A) shows a heavily calcified plaque with blooming artifacts (white arrow) in the proximal left anterior descending artery with obstructive stenosis. Invasive coronary angiography (B) demonstrates a 26%-50% stenosis, and Fractional Flow Reserve was 0.89, in contrast to the report of CT-FFRAI that predicts FFR ≤ 0.8 (C). Of note, the patient also had an obstructive stenosis on the left circumflex artery with CT-FFRAI > 0.8 prediction and invasive Fractional Flow Reserve > 0.8 (FFR = 0.91).Peters et al; European Radiology
False-positive case. A representative case of an 81-year-old male patient with a recent onset of stable chest pain. Curved multiplanar reconstruction coronary computed tomography angiography (A) shows a heavily calcified plaque with blooming artifacts (white arrow) in the proximal left anterior descending artery with obstructive stenosis. Invasive coronary angiography (B) demonstrates a 26%-50% stenosis, and Fractional Flow Reserve was 0.89, in contrast to the report of CT-FFRAI that predicts FFR ≤ 0.8 (C). Of note, the patient also had an obstructive stenosis on the left circumflex artery with CT-FFRAI > 0.8 prediction and invasive Fractional Flow Reserve > 0.8 (FFR = 0.91).Peters et al; European Radiology
While FFR measured during invasive coronary angiography (ICA) is endorsed in guidelines for predicting vessel-specific coronary ischemia, there has been increased focus on the development of noninvasive approaches. Estimating FFR from computational fluid dynamics (CFD) simulations using CCTA is now an established approach for diagnosis and management in patients with intermediate risk and stable chest pain, the authors explained.
The deep-learning model evaluated in the study was trained on CCTA images labeled with FFR values measured during ICA. CT-FFRAI is structured around several intermediate models, each dedicated to a specific function, which refines the analysis, they noted. The model, which uses nine cMPR images as input and classifies coronary lesions as either CT-FFRAI ≤ 0.8 or > 0.8, learns the relationship between the coronary anatomy and FFR directly from the images and integrates anatomical and functional data through advanced deep-learning methods.
 Peters et al; European Radiology
Peters et al; European Radiology
The researchers retrospectively selected all consecutive patients between 2017 and 2022 at the two centers who had undergone CCTA and had a coronary stenosis ≥ 50% on the initial reading, followed by ICA with invasive FFR and/or iFR pressure measurement during ICA within three months. A total of 275 patients were included in the study; the cohort included 187 men and 88 women, with a mean age of 66 years (age range, 37-91 years).
CCTA had been performed based on stable chest pain or equivalent symptoms in patients with a moderate likelihood of obstructive coronary artery disease, the authors wrote. The study team did not include vessels without invasive pressure measurement in their analysis; 322 vessels were included from the 275 patients.
A senior and junior radiologist at each center supervised the vessel centerline generation and windowing parameters, with the ability to make manual adjustments as they deemed necessary. cMPR images were then uploaded to a server-based module for CT-FFRAI processing. The images were subsequently analyzed to assess the diagnostic performance of CT-FFRAI by the radiologists.
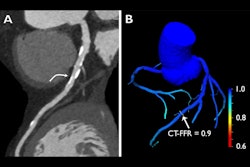
 True-negative case. A representative case of a 60-year-old female patient with a recent onset of stable chest pain. Curved multiplanar reconstruction coronary computed tomography angiography (A) shows a soft plaque at the middle portion of the right coronary artery with obstructive stenosis (white arrow). Invasive coronary angiography (B) confirms a 26%–50% stenosis (white arrow). The Fractional Flow Reserve measurement was 0.94, which is above the 0.8 threshold. Instantaneous wave-Free Ratio measurement was 0.95, which is above the 0.89 threshold. The CT-FFRAI prediction was > 0.8 (C).Peters et al; European Radiology
True-negative case. A representative case of a 60-year-old female patient with a recent onset of stable chest pain. Curved multiplanar reconstruction coronary computed tomography angiography (A) shows a soft plaque at the middle portion of the right coronary artery with obstructive stenosis (white arrow). Invasive coronary angiography (B) confirms a 26%–50% stenosis (white arrow). The Fractional Flow Reserve measurement was 0.94, which is above the 0.8 threshold. Instantaneous wave-Free Ratio measurement was 0.95, which is above the 0.89 threshold. The CT-FFRAI prediction was > 0.8 (C).Peters et al; European Radiology
The accuracy of CT-FFRAI in predicting invasive FFR ≤ 0.8 and invasive iFR ≤ 0.89 with the senior radiologists’ centerline-building supervision was 83% (186 out of 224) and 83% (197 of 238), respectively; for junior radiologists, the respective percentages were 79% (177 of 224) and 78% (186 of 238). The difference in diagnostic accuracy of CT-FFRAI between senior and junior radiologists’ supervision was not significant (p = 0.327).
For lesions assessed with both invasive FFR and iFR (a total of 140), the accuracy rates for senior radiologist-supervised CT-FFRAI were 85% (119 of 140) and 80.7% (113 of 140), respectively, comparable to those observed in the overall cohort. There was discordance in 11% of cases (16 of 140) between invasive FFR and iFR measurements, defined as FFR ≤ 0.8 and iFR > 0.89 (in 7 cases) or FFR > 0.8 and iFR ≤ 0.89 (9 cases). For this group, the CT-FFRAI (as supervised by senior radiologists) agreed with FFR in 69% (11 of 16) and with iFR in 31% (5 of 16) of cases.
However, unsupervised CT-FFRAI had much lower diagnostic accuracy: 61% (136 of 224) and 62% (148 of 238) compared with invasive FFR and iFR, respectively (p < 0.001). Due to the increase in false-positive cases, there was notably lower specificity and PPV, the authors noted.
Among factors that could influence the performance of the model, only the calcium score of the stenotic vessel had a significant detrimental effect on the diagnostic accuracy of CT-FFRAI prediction of vessel-specific ischemia.
The authors pointed out that this study uses a much larger population than previous studies of the CT-FFRAI model’s performance, with other aspects that improve the study design. “The model’s reliability was demonstrated by a similar diagnostic performance using datasets from two different CT scanners, encompassing both prospective and retrospective scanning modes, and by substantial observer concordance between supervisors of different levels of experience.”
Read the study on the European Radiology website.