New analysis of firearm injuries shows that forensic radiology training substantially enhances postmortem CT (PMCT) reliability and enables radiologists to recognize injury patterns, authors noted in an article posted on 24 October in La Radiologia Medica, the official journal of the Italian Society of Medical and Interventional Radiology (SIRM).
“Radiologists with forensic expertise are significantly more accurate in identifying firearm-related injuries, particularly entry and exit wounds, than those without specific training,” Dr. Maria Grazia Fornasari, from the Radiology Department at the University of Palermo, and colleagues wrote. “These findings support the growing recognition of PMCT as a valuable tool in forensic investigations.”
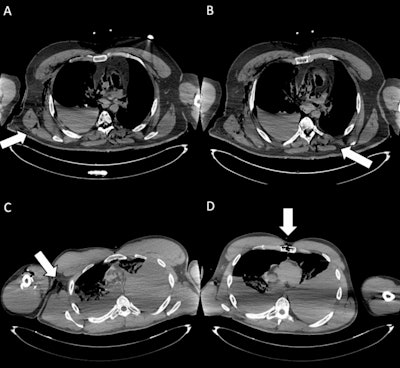 Entry wounds. (A) Axial CT scan shows an entrance wound in the right posterior thoracic wall (white arrow), with adjacent soft-tissue disruption and subcutaneous gas, consistent with a penetrating gunshot injury. (B) Axial CT image depicts the ballistic trajectory with paravertebral left soft-tissue damage (white arrow) and subcutaneous emphysema in the posterior right chest wall. (C) Cross-sectional CT slice demonstrates an entrance wound at the root of the right arm (white arrow), associated with soft-tissue laceration and subcutaneous emphysema. (D) CT image illustrates an entrance wound at the sternal level (white arrow), with anterior chest wall disruption and surrounding soft-tissue alterations, compatible with penetrating trauma. The identification of entrance gunshot wounds showed only moderate inter-reader agreement (Fleiss’ kappa = 0.55). In particular, less forensic-experienced readers demonstrated markedly reduced sensitivity (29.7%), highlighting the diagnostic challenges of detecting these findings on postmortem CT.All figures courtesy of Dr. Maria Grazia Fornasari, Dr. Giuseppe Lo Re, Dr. Roberto Cannella et al and La Radiologia Medica/SIRM.
Entry wounds. (A) Axial CT scan shows an entrance wound in the right posterior thoracic wall (white arrow), with adjacent soft-tissue disruption and subcutaneous gas, consistent with a penetrating gunshot injury. (B) Axial CT image depicts the ballistic trajectory with paravertebral left soft-tissue damage (white arrow) and subcutaneous emphysema in the posterior right chest wall. (C) Cross-sectional CT slice demonstrates an entrance wound at the root of the right arm (white arrow), associated with soft-tissue laceration and subcutaneous emphysema. (D) CT image illustrates an entrance wound at the sternal level (white arrow), with anterior chest wall disruption and surrounding soft-tissue alterations, compatible with penetrating trauma. The identification of entrance gunshot wounds showed only moderate inter-reader agreement (Fleiss’ kappa = 0.55). In particular, less forensic-experienced readers demonstrated markedly reduced sensitivity (29.7%), highlighting the diagnostic challenges of detecting these findings on postmortem CT.All figures courtesy of Dr. Maria Grazia Fornasari, Dr. Giuseppe Lo Re, Dr. Roberto Cannella et al and La Radiologia Medica/SIRM.
The researchers examined 10 firearm fatalities (8 homicides, 2 suicides) between January 2021 and August 2024. The sample included individuals between the ages of 25 and 66 (8 men, 2 women), with injuries from both short- and long-barrel firearms. PMCT scans were performed at Policlinico Paolo Giaccone in Palermo 24 hours before the autopsy, ensuring optimal temporal correlation between radiological imaging and anatomical-pathological findings. For all cases, the postmortem investigation of the included cases was less than 72 hours.
Four radiologists with varying forensic experience analyzed the PMCT scans: an experienced forensic radiologist, an experienced clinical radiologist without forensic training, a radiology resident with forensic training, and a radiology resident without forensic expertise.
The team evaluated 960 anatomical findings categorized by lesion type. Among these, 150 cases (15.6%) involved organ-related injuries, while 230 cases (24%) were associated with fractures. Additionally, 40 findings (4.2%) were related to vascular damage, and 50 cases (5.2%) involved hemorrhages. Firearm injuries constituted a significant portion of the dataset, with 220 cases (22.9%) of entry wounds, 190 cases (19.8%) of exit wounds, and 80 instances (8.3%) of retained bullets.
“This comprehensive dataset enabled a detailed comparison of reader performance across different lesion types, highlighting the impact of forensic training on diagnostic accuracy,” the authors wrote.
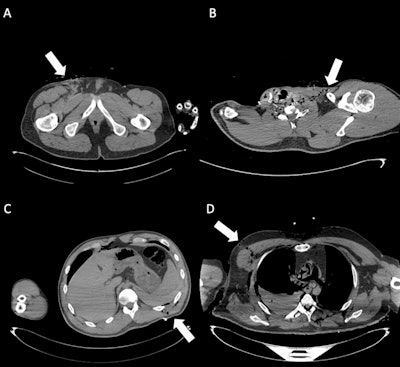 Exit wounds. (A) Axial CT scan shows an exit wound in the subcutaneous soft tissues at the root of the right thigh (white arrow). (B) Axial CT image depicts an exit wound in the left supraclavicular region (white arrow), visible as a focal soft-tissue defect with surrounding gas bubbles. (C) Cross-sectional CT slice illustrates an exit wound at the left posterior abdominal wall (white arrow), with subcutaneous emphysema and adjacent soft-tissue disruption. (D) CT image demonstrates an exit wound in the right chest region (white arrow), characterized by soft-tissue laceration and subcutaneous gas. Exit gunshot wounds were associated with the lowest inter-reader agreement (Fleiss’ kappa = 0.36). Despite the very high specificity of virtopsy, sensitivity was particularly low among readers without forensic experience (12.5% and 16.7%), underlining the difficulty in correctly identifying these injuries on postmortem CT.
Exit wounds. (A) Axial CT scan shows an exit wound in the subcutaneous soft tissues at the root of the right thigh (white arrow). (B) Axial CT image depicts an exit wound in the left supraclavicular region (white arrow), visible as a focal soft-tissue defect with surrounding gas bubbles. (C) Cross-sectional CT slice illustrates an exit wound at the left posterior abdominal wall (white arrow), with subcutaneous emphysema and adjacent soft-tissue disruption. (D) CT image demonstrates an exit wound in the right chest region (white arrow), characterized by soft-tissue laceration and subcutaneous gas. Exit gunshot wounds were associated with the lowest inter-reader agreement (Fleiss’ kappa = 0.36). Despite the very high specificity of virtopsy, sensitivity was particularly low among readers without forensic experience (12.5% and 16.7%), underlining the difficulty in correctly identifying these injuries on postmortem CT.
Results showed significantly higher diagnostic accuracy among radiologists with forensic training, particularly in detecting entrance and exit wounds, as well as organ injuries. The most experienced forensic radiologist achieved the highest overall accuracy, with an area under the curve (AUC) of 0.9 (95% confidence interval [CI] 0.887-0.916), followed by the radiology resident with forensic experience, who obtained an AUC of 0.86 (95% CI 0.839-0.883).
In contrast, the radiologist with clinical but no forensic training and the radiology resident without forensic experience had lower AUC values, both reaching 0.76 (95% CI 0.727-0.783).
Although the specificity of PMCT evaluation remained consistently high across all readers (over 99%), sensitivity varied significantly depending on the reader’s experience. Readers without forensic expertise showed low sensitivity in detecting key findings.
For organ injuries, sensitivity was only 31% for the radiologist with clinical but no forensic training and 51.7% for the radiology resident without forensic experience. Similarly, for firearm entry wounds, both the doctors without training had a sensitivity of 29.7%, while for exit wounds, their sensitivity was even lower, at 12.5% for the radiologist with clinical but no forensic training and 16.7% for the radiology resident without forensic experience.
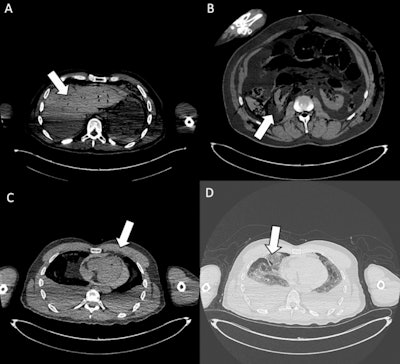 Organ injuries. (A) Axial CT scan shows traumatic injury to the bi-lobar liver parenchyma (white arrow). Moderate postmortem decomposition is also evident, with heterogeneous intraparenchymal gas distribution. (B) Cross-sectional CT image demonstrates a laceration of the right kidney (white arrow), consistent with penetrating trauma. (C) Axial CT slice shows a pericardial lesion (white arrow), with small gas bubbles in the anterior pericardial region, indicative of traumatic pericardial injury. (D) CT image highlights a laceration of the right middle lobe (white arrow), associated with pulmonary contusion, omolateral pneumothorax, and bilateral pleural effusion. In the assessment of organ injuries, inter-reader agreement was only moderate (Fleiss’ kappa = 0.52). Sensitivity was again limited among less forensic-experienced readers (31% and 51.7%), reflecting the interpretative complexity and reduced diagnostic accuracy of postmortem CT in this setting.
Organ injuries. (A) Axial CT scan shows traumatic injury to the bi-lobar liver parenchyma (white arrow). Moderate postmortem decomposition is also evident, with heterogeneous intraparenchymal gas distribution. (B) Cross-sectional CT image demonstrates a laceration of the right kidney (white arrow), consistent with penetrating trauma. (C) Axial CT slice shows a pericardial lesion (white arrow), with small gas bubbles in the anterior pericardial region, indicative of traumatic pericardial injury. (D) CT image highlights a laceration of the right middle lobe (white arrow), associated with pulmonary contusion, omolateral pneumothorax, and bilateral pleural effusion. In the assessment of organ injuries, inter-reader agreement was only moderate (Fleiss’ kappa = 0.52). Sensitivity was again limited among less forensic-experienced readers (31% and 51.7%), reflecting the interpretative complexity and reduced diagnostic accuracy of postmortem CT in this setting.
These findings underscore the critical role of forensic radiology training in enhancing PMCT reliability, Fornasari and colleagues pointed out. Also, standardized reporting protocols and structured training programs are crucial for strengthening medicolegal investigations, thereby ensuring accurate and reproducible forensic imaging assessments.
By fostering interdisciplinary collaboration and investing in technology, forensic radiology can continue to evolve as a crucial tool in modern forensic medicine, the researchers wrote. “Forensic radiology training not only improves diagnostic accuracy but also equips radiologists with the ability to recognize injury patterns specific to firearm-related fatalities, differentiate true lesions from postmortem artifacts, and apply medicolegal standards in structured reporting.”
Future research should explore advanced imaging techniques, including radiomics and AI-driven analysis, to optimize forensic radiology practices, they concluded.
You can read the full journal article here.





















