Fear can lead to avoidance of lung cancer screening, but a welcome boost has come from a new study analyzing the long-term effects of low-dose CT (LDCT) examinations in the U.K. Lung Cancer Screening trial (UKLS). It found that patients randomized to the imaging arm did not experience unnecessary long-term anxiety.
The authors of the study, published in Thorax on 28 July, insist the impact of incidental findings during screening warrants additional research, but the first study looking at psychosocial outcomes of the UKLS trial adds to the growing volume of evidence supporting implementation of national programs for routine screening.
"There is currently no screening program for lung cancer in the U.K., so this evidence is important for policymakers deciding whether to introduce CT lung cancer screening for high-risk groups, and for clinicians who may be involved in planning and delivering it as a service if it becomes routinely available in the future," lead author Kate Brain, a health psychologist at the College of Biomedical and Life Sciences in Cardiff University, told AuntMinnieEurope.com in an email.
 Kate Brain is a health psychologist at Cardiff University.
Kate Brain is a health psychologist at Cardiff University.She found CT screening did not cause undue worry or anxiety when high-risk participants were followed up over a two-year period, and although those who needed to have a repeat scan reported slightly higher cancer distress, this effect was only temporary.
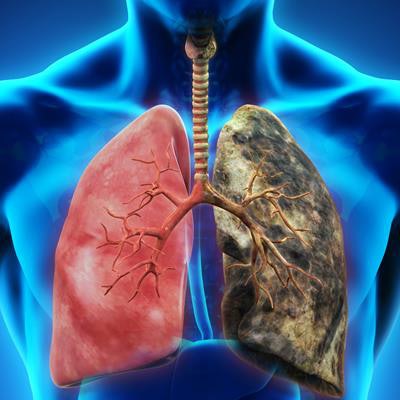
Lung cancer kills almost 40,000 people per year in the U.K., and that's partly because around 75% of patients are diagnosed at a late stage when there are fewer treatment options, explained Brain and colleagues. Although the five-year survival rate for lung cancer in the U.K. is improving, at 10%, it is still lower than in other countries with comparable healthcare systems and the disease remains the leading cause of cancer-related mortality in the country.
Specifically, 65% of cases are diagnosed at stage III or stage IV when treatment is usually palliative. Early detection through screening strategies including LDCT improve the odds of survival, but fear and stigma, as well as fatalistic beliefs and avoidant behavior, remain barriers to screening, and probably more so in poorer areas where lung cancer incidence and mortality are higher, they noted.
While there is positive evidence from the U.S National Lung Cancer Screening Trial (NLST) for the effectiveness of LDCT screening in detecting early-stage lung cancer among high-risk groups, its feasibility must be thoroughly tested in the U.K., and this includes evaluating the psychosocial harms and benefits of CT lung cancer screening in high-risk patients, Brain stated.
European comparisons
The results of this study analyzing psychosocial effects of the LDCT UKLS trial are in line with those from the Dutch/Belgian NELSON (Nederlands-Leuvens Longkanker Screenings Onderzoek) trial and the Danish Lung Cancer Screening Trial (DLCST), which found no differential effect of trial allocation on a range of psychosocial outcomes at one year and two years follow up. Similarly, the NLST showed no significant differences between those receiving an abnormal lung-screening result and those receiving normal results in anxiety and health-related quality of life at one and six months follow-up.
"Overall, the results confirm those of previous trials that any adverse psychosocial effects are short-lived and not clinically significant. But further research is needed into the impact of receiving a significant incidental finding, because there may be a higher rate of such findings if CT screening is rolled out in routine clinical practice compared with what we would see in a controlled trial setting," she said.
The study took place across six recruitment centers, three in the northwestern county of Merseyside and three across the more affluent counties of Cambridgeshire and Bedfordshire. This sampling approach led to good representation of participants from lower and higher socioeconomic groups, according to Brain, adding that the authors expected deprivation would be linked to poorer psychosocial outcomes.
Individuals between the ages of 50 and 75 were contacted via primary care and filled in a baseline questionnaire (T0). From these responses, 4,037 participants were identified as being at high risk of developing lung cancer and these individuals were then randomized to the two different trial pathways: 2,018 were sent to LDCT screening (intervention) while 2,019 went to usual care/no screening (control).
Questionnaires (T1) measuring cancer distress, anxiety, depression, and decision satisfaction were sent two weeks after baseline scan results or two weeks following assignment to the control group. T2 questionnaires measuring the same emotional responses were sent up to two years after recruitment.
Cancer distress was higher at T1 in the intervention arm, who received positive screening results, but not at T2, showing that any stress from screening was temporary. Conversely, anxiety and depression were higher in the control arm at T2 although this was deemed not clinically relevant. Furthermore, fewer control than screened participants were satisfied with their decision to participate in UKLS.
The study also revealed cancer distress was higher in women, participants younger than 65 years old, current smokers, those with lung cancer experience, and those recruited from the Liverpool area in Merseyside, regardless of whether they were assigned to the screening or control group.
"Further studies -- especially those involving in-depth qualitative methods -- would be very useful in increasing our understanding of psychosocial responses to CT lung cancer screening in these groups. For example, it would be useful to explore women's perceptions and beliefs about lung cancer screening, in comparison with breast and cervical screening programs, which are routinely available in the U.K. National Health Service," Brain noted.
She leads a research program looking at the broader psychosocial aspects of cancer screening, prevention, and early diagnosis. Her group intends to carry out further studies into perceptions and beliefs about lung cancer early detection in high-risk, harder-to-reach groups.
"Fear can lead to avoidance of lung screening, but an important message is that finding lung cancer early means there is a better chance of survival. Further research is needed to develop and evaluate lung screening invitation strategies and information materials that are targeted at high-risk groups who may be less likely to take part, or experience worry when they do take part in CT lung cancer screening," she concluded.



















