Using fractional flow reserve CT (FFR-CT) to assess the severity of coronary disease at CT angiography offers powerful advantages in daily clinical practice, but to use it optimally, practitioners must create a place for the noninvasive procedure in their practices and know when to stay away, according to a Dutch expert.
Multiple studies have confirmed FFR-CT's utility in assessing the severity of stenosis detected at coronary CT angiography (CCTA). CCTA alone is great for ruling out coronary disease, of course, but it has limitations for assessing the severity of stenosis, often overcalling the degree of flow impairment. To determine the hemodynamic significance of lesions, FFR-CT compares strongly to competing exams when it is used correctly, said Dr. Koen Nieman, PhD, from Rotterdam University Medical Center.
"CT angiography is an excellent technique to rule out coronary artery disease, but it overestimates angiographic stenosis whether invasive or noninvasive," he told delegates at the 2016 International Symposium on Computed Tomography (ISCT 2016), adding that CCTA also routinely overestimates the hemodynamic severity of lesions.
"We need something extra to make the exam a complete exam," he said. If not FFR-CT, "we can go to the cath lab for invasive fractional flow reserve, or just do a catheterization ... We can do stress perfusion imaging."
Measuring blood flow
The mechanism of the algorithm rests on a very physiologic concept, Nieman said. When processed on a powerful computer one can use CT images to calculate the pressure in the vessel wall during vasodilation. The algorithm uses flow dynamics computations to calculate resting blood flow from left ventricular mass and resistance from the vessel diameter measurements, repeating the process after simulating resistance with adenosine stress.
With the results of several strong trials under its belt, FFR-CT has proven its utility, he noted. For example, the multicenter Prospective Longitudinal Trial of FFR-CT: Outcome and Resource Impacts [PLATFORM] trial (Douglas et al, 2015) looked at 584 stable chest pain patients in 11 European centers who were scheduled for invasive coronary angiography. The investigators found the use of FFR-CT could obviate the need for invasive tests such as angiography in as many as 61% of patients.
Among patients who underwent invasive angiography, 73% of those in a group assigned to usual care had negative results, versus just 12.4% of those who had undergone FFR-CT before invasive angiography, Nieman said.
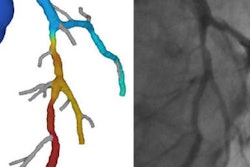
In the Analysis of Coronary Blood Flow using CT Angiography: Next Steps (NXT) trial (Norgaard et al, April 2014) FFR-CT showed sensitivity of 83% to 84% and specificity of 60% to 80%, with accuracy of 65% to 68% in 254 patients scheduled to undergo invasive coronary angiography. The authors concluded FFR-CT provides high diagnostic accuracy and discrimination for the diagnosis of hemodynamically significant coronary artery disease using invasive FFR as the reference standard. Perhaps most impressive, FFR-CT reclassified 68% of false positives at CCTA as normal.
"FFR-CT has the ability to remove the false positives that we create," he said. "False-positive means we would send more than 50% of those patients to the cath lab because we think the patient has obstructive coronary disease. But if you do FFR it will turn out negative and you don't have to send them to the cath lab and you will avoid invasive angiography and potential revascularizations -- that was the goal and that's what this trial proved."
Clinical considerations
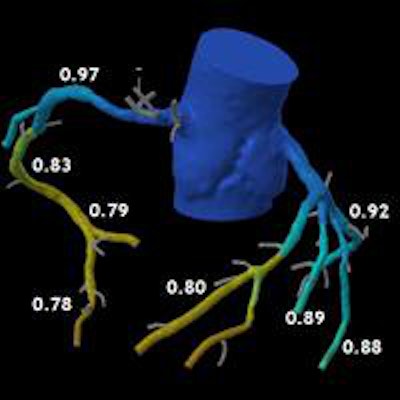
The Heartflow software used by Nieman's group in Rotterdam makes a lot of calculations, and ultimately displays the coronaries in a colorful 3D tree where blue indicates patent arteries and orange and yellow reveal hemodynamic obstruction.
"Once you have a 3D model you can actually sample that model right on the coronary tree and you can define where is the greatest jump in FFR is," he said. The group is increasingly using the technique in patients with significant calcifications in circumflex and left anterior descending arteries.
"We can take a gamble and say it's probably not clinically significant -- or we can do FFR-CT and it will turn out that all the coronaries are nice and blue and don't have any hemodynamic abnormalities," he said of one example.
Another FFR-CT case revealed significant flow restrictions, but not in the area surrounding the lesion where they matter. The young man in his mid-40s had atrial fibrillation and plaque stretching from a proximal left anterior descending artery stenosis > 50%.
 Coronary CT angiography revealed stenosis > 50% in a mid-40s man with atrial fibrillation. However, FFR-CT showed no flow restrictions (depicted in blue) in the area surrounding the calcifications, only minor flow restrictions (yellow and red) in the distal arteries, enabling the patient to be managed conservatively. Image courtesy of Dr. Koen Nieman.
Coronary CT angiography revealed stenosis > 50% in a mid-40s man with atrial fibrillation. However, FFR-CT showed no flow restrictions (depicted in blue) in the area surrounding the calcifications, only minor flow restrictions (yellow and red) in the distal arteries, enabling the patient to be managed conservatively. Image courtesy of Dr. Koen Nieman."This patient would be very easy to send to the cath lab, and most people would do that or more -- but the interesting thing was that FFR-CT as calculated did not find any significant drop in FFR over the lesions," Nieman said. As a result, the patient could be managed conservatively.
In patients such as these who have plaque and calcium in the arteries, peripheral lesions often show FFR-CT values below 0.08, indicating hemodynamic significance in the small vessels. But FFR-CT readings fall to normal levels around the lesion (FFR 0.97 to 0.83 in this case), clearing the way for noninvasive management with medication, Nieman said.
What to consider before FFR-CT?
- Good image quality is essential. Misalignment artifacts in particular can actually cause false positives.
- Use beta-blockers, nitroglycerine, and follow Society of Cardiac Computed Tomography (SCCT) guidelines to obtain the best possible image quality.
- Most calcifications won't hurt the exam, but some larger ones can preclude its use, Nieman said.
- Reconstructions are important. Think about what to use before performing FFR-CT.
- Heartflow software cannot process datasets with only systolic images
"This is something that we had to get used to, because we frequently scan patients only during systole, but probably that will change in the future," Nieman said.
Importantly, the populations studied to date have been fairly narrow -- generally patients with normal hearts, no congenital heart disease, no myocardial infarction, no revascularizations, no coronary artery bypass grafts (CABG), no cardiomyopathies, he continued. "These patients have not been evaluated [with FFR-CT] and it may not even be possible."
In the medical facility, it takes time to convince colleagues that this test is worthwhile, and affordable. You will need to show them the results, convince them, and find a way to incorporate the costs of FFR-CT into the practice, Nieman said. But what is known so far is positive.
"We can see it's accurate, we can see it may reduce the number of resvascularizations performed," he said.
New and next steps
A new development in FFR-CT is the ADVANCE registry, led by Dr. Jonathan Leipsic at the University of British Columbia, Vancouver. The planned 5,000-patient registry will collect data on how FFR-CT performs in clinical practice, look at clinical outcomes, and see reclassification rates and the number of nonassessible cases in FFR-CT, he said, "and it will be very interesting to see how the technique will perform in the real world."
Finally, an alternative FFR-CT algorithm by Siemens Healthineers has shown similar results to Heartflow is now being evaluated at sites in Korea, Poland, and Sweden, to assess its suitability for FFR-CT.
"In summary, FFR-CT is accurate in comparison to invasive FFR-CT, and avoids overestimation of lesion severity, potentially avoids invasive catheterization," he said, adding that more research is needed in the implementation and performance of FFR-CT in clinical practice, particularly in comparison with other noninvasive diagnostic strategies.