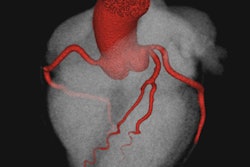
ROME - In patients with chest pain, should you use cardiac CT or functional testing? A large study from Denmark presented on Monday at the European Society of Cardiology (ESC) annual congress found advantages and disadvantages to the cardiac CT-based approach.
In nearly 87,000 patients treated for suspected coronary artery disease over a seven-year period, the use of cardiac CT as an initial test was associated with higher costs and more use of additional downstream testing such as catheterization. But patients in the cardiac CT group also tended to have lower rates of cardiac events later on.
 Back home from California, Mads Emil Jørgensen presented his group's data at ESC 2016.
Back home from California, Mads Emil Jørgensen presented his group's data at ESC 2016."There has been some controversy surrounding this," lead author Mads Emil Jørgensen, from the Cardiovascular Research Center at Herlev-Gentofte Hospital at the University of Copenhagen, told AuntMinnieEurope.com. "Cardiac CT has been taking over from stress tests, including exercise ECGs and SPECT scans."
Jørgensen and his colleagues looked at whether the choice of test modality, in patients referred with suspected coronary artery disease, affects downstream patient management, and subsequently, long-term risks of adverse events and death. They retrieved national data on tests, procedures, drug use, and in-hospital diagnosed comorbidities, and evaluated changes in pharmacotherapy, further testing, and the need for revascularization within 120 days.
The team identified nearly 86,705 patients without cardiac disease who underwent first-time noninvasive cardiac testing between 2009 and 2015. Of these, 53,744 had stress tests and 32,961 had cardiac CT. The mean age in both groups was 57.4, and 48.8% of those in the stress test group were men, compared with 45% in the cardiac CT group.
The key data are shown in the two tables. Also, the use of catheterization, percutaneous coronary intervention, and coronary artery bypass grafting was significantly higher following cardiac CT, and the proportion of patients having coronary revascularization, if undergoing catheterization, was highest after initial cardiac CT.
| Changes in statin and aspirin therapy after cardiac CT | |||||
| Medication changes within 120 days | Changed medication* | ||||
| Initiated | Discontinued | % | p-value | ||
| Statin | Cardiac CT | 15.9 | 5.4 | 21.3 | |
| Stress test | 9.1 | 4.3 | 13.4 | < 0.05 | |
| Aspirin | Cardiac CT | 12.7 | 12.2 | 24.9 | |
| Stress test | 8.5 | 7.5 | 16.0 | < 0.05 | |
| Beta-blocker | Cardiac CT | 6.5 | 4.9 | 11.4 | |
| Stress test | 7.9 | 3.5 | 11.4 | 0.88 | |
Use of further testing was equally frequent between the two groups. However, noninvasive testing was preferred after initial stress test, while catheterization was preferred after initial cardiac CT.
| Use of further testing after initial stress test and cardiac CT | |||
| Further testing within 120 days | |||
| Initial stress testing | Initial cardiac CT | p-value | |
| No further testing | 42,662 (79.4) | 26,165 (79.4) | 1.00 |
| Noninvasive only | 5,655 (10.5) | 1,941 (5.9) | < 0.05 |
| Cath only | 4,292 (8.0) | 4,265 (12.9) | < 0.05 |
| Noninvasive + cath | 1,135 (2.1) | 590 (1.8) | < 0.05 |
Overall, Jørgensen and colleagues found the following:
- Mean costs, including initial testing, repeated tests, invasive procedures, drug use, and hospitalization for acute coronary syndrome events were $948 (850 euros) for stress testing and $1,250 (1120 euros) for cardiac CT, representing a 32% difference.
- More frequent use of invasive procedures was the main reason for increased costs within 120 days after initial cardiac CT.
- The proportion of patients undergoing revascularization after diagnostic catheterization was higher after initial cardiac CT than initial stress testing, suggesting that catheterization is not overused following cardiac CT.
- For all-cause mortality, 2,131 events (4%) occurred in the stress test group, compared with 699 (2.1%) in the cardiac CT group. The figures for cardiovascular deaths were 506 (1%) in the stress test group, against 152 (0.6%) in the cardiac CT patients, and the number of acute coronary syndrome (ACS) events was 1,324 (2.5%) in the stress group and 536 (1.6%) in the cardiac CT group.
For the study, Jørgensen was supported by the Lundbeck Foundation Clinical Research Fellowship Program, of which he is a candidate for fellowship. As part of the fellowship, he was based at the department of health research and policymaking at Stanford University in California between May 2015 and February 2016.
"It was a great experience and opportunity, and that was when we did most of the work on the chest pain study," he said. The next stage is to get more recognition and awareness for the team's research, and hopefully publication in a peer-review journal, he added.