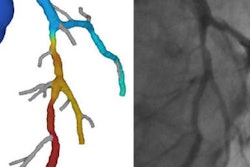
The key question surrounding the functional significance of a coronary lesion can be answered with absolute lesion diameter rather than percent stenosis as measured with coronary CT angiography (CCTA), concludes a new study in European Radiology.
Investigators found that absolute, rather than relative, lumen diameters on CCTA scans were best correlated with functional parameters at angiography, and could therefore be used in decision-making about coronary intervention, according to an article in the November issue (European Radiology, November 2016, Vol. 26:11, pp. 3781-3789).
The team from Medical University of Vienna and Innsbruck University in Austria retrospectively studied 160 patients referred for CCTA who also underwent invasive coronary angiography. The results showed absolute lumen diameter was a bigger predictor than percentage stenosis of the lumen -- the conventional assessment method -- for assessing coronary function based on invasive angiography results.
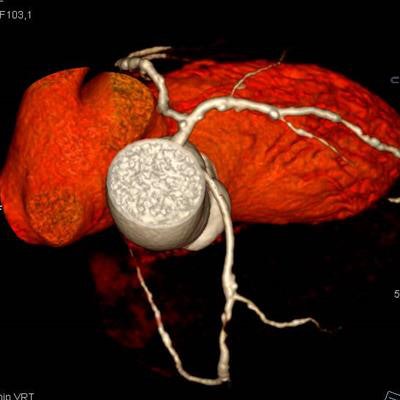
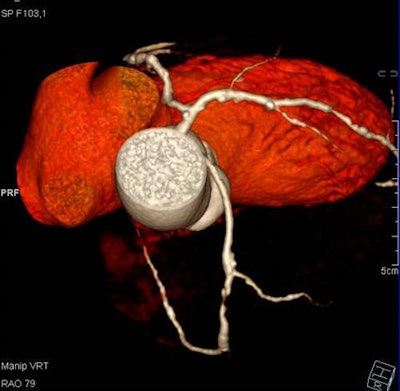 Fifty-three year-old male with acute chest pain. CCTA reveals a mean lumen area of 1.9 mm3, 80% area, 55% diameter stenosis, and anomalous right coronary artery arising from the left coronary sinus. Image courtesy of Dr. Gudrun Feuchtner.
Fifty-three year-old male with acute chest pain. CCTA reveals a mean lumen area of 1.9 mm3, 80% area, 55% diameter stenosis, and anomalous right coronary artery arising from the left coronary sinus. Image courtesy of Dr. Gudrun Feuchtner."Absolute lumen area was more accurate than percent of stenosis," wrote co-author Dr. Gudrun Feuchtner in an email, cautioning the results apply only to proximal coronary segments.
Quantitative coronary CTA "is accurate for the prediction of functional relevant stenosis," wrote lead author Dr. Fabian Plank and colleagues. Plank was responsible for most of the image analysis work, Feuchtner said.
CT often the only test
The fact that some 40% of individuals undergoing coronary CT angiography do not undergo further intervention is meaningful, they wrote. CCTA is a powerful noninvasive tool for ruling out significant stenosis and detecting coronary atherosclerosis, and it is an excellent gatekeeper for invasive coronary angiography, they said.
But despite an excellent 97% negative predictive value (NPV), CCTA's positive predictive value (PPV) is only moderate and needs improvement. Visual grading of stenosis is how CCTA is typically interpreted to define further patient management. After CCTA, generally:
- Patients with mild (< 50 %) stenosis by CCTA undergo risk factor modification.
- Patients with intermediate (50% to 70%) coronary stenosis are referred for myocardial perfusion SPECT.
- Patients with severe coronary stenosis at CCTA are referred for invasive angiography.
"This classification is subjective, observer-dependent, and influenced by a variety of factors such as individual reading skill level," Plank and colleagues wrote. But the actual measurements are available and may be better.
Quantitative coronary vessel and luminal stenosis parameters acquired at CCTA include absolute cross-sectional vessel area, diameter, and relative percentage area and percentage diameter stenosis. These measurements are well correlated with intravascular ultrasound -- better, in fact, than they are correlated with angiography, the team wrote.
Little evidence on CT's predictive power
The use of quantitative CCTA to predict the functional significance of a coronary lesion is not well defined. Previous studies have included fewer than 100 patients.
Still, the "accurate assessment of a lesion's functional significance (i.e., flow-limiting lesion) is of paramount importance in defining further patient management, because a major trial showed that only flow-limiting lesions with a fractional flow reserve (FFR) of < 0.8 benefit from consecutive coronary revascularization procedures," wrote the authors.
How well does lumen size correlate with function at angiography? In 200 patients undergoing CCTA, measurements of absolute vessel parameters included minimum lumen area (MLA), minimum lumen diameter (MLD), relative percentage of lumen area and diameter stenosis, and lesion length to predict flow-limited stenosis by invasive coronary angiography requiring coronary revascularization.
Included were the right coronary artery, left anterior descending artery, and circumflex arteries with a vessel area of 5 mm and later, and visually inspected high-grade stenosis seen on CTA during routine clinical readouts within three weeks, that were estimated to occupy 50% to 70% of the vessel lumen diameters.
Chart review, review of previous studies, and telephone follow-up were conducted after the scans. Patients were excluded for previous percutaneous coronary intervention, myocardial infarction, or coronary artery bypass grafting.
After contrast injection, patients were scanned with a 64-detector-row CT scanner (Somatom Sensation, Siemens Healthineers) before December 1999 and with a 128-detector-row dual-source CT scanner (Somatom Definition Flash, Siemens Healthineers) thereafter. The reference standard was invasive coronary artery obstruction of 70% stenosis, and fractional flow reserve of 0.8. A total of 210 coronary segments were analyzed, 59% of which were positive for stenosis.
Mean lumen area (MLA) was defined as the optimal cutoff (0.001) with a sensitivity of 90.9% and specificity of 89.3% for functional relevant stenosis. The optimal mean cutoff for the mean lumen diameter was 1.2 mm (p = 0.001). An experienced observer interpreted the results.
Beats percent stenosis
Mean lumen area ≤ 1.8 mm2 and mean lumen diameter ≤ 1.2 mm were the most accurate cutoffs for prediction of hemodynamically significant stenosis by invasive coronary angiography, with higher accuracy than relative percent stenosis, Plank and colleagues wrote.
"Our study shows superiority of absolute vessel lumen quantitative parameters (MLA, MLD, and LL/MLA ratio) with a higher accuracy for prediction of hemodynamically relevant flow-limiting coronary stenosis requiring coronary revascularization, as compared relative percentage area and diameter stenosis," the authors wrote. "The MLA was the most powerful parameter, aside from the MLD and the LL/MLA ratio."
The MLA cut-off of 1.8 mm2 was in line with a paper by Rossi et al in their study of fewer than 100 patients. The greatest sensitivity was found at 2.1 mm2 MLA. If the MLA ranges within 1.8 and 2.1 mm2, significant stenosis is possible and a myocardial ischemia test is recommended, the group wrote.
Of note, absolute lumen diameter was identified as a value parameter for the prediction of high-grade stenosis at angiography. Absolute diameter sizing is more susceptible to variations than absolute lumen tracing, because the stenotic vessel lumen is often noncircular and oval shaped due to a single-side plaque, leading to greater interobserver variability.
The relative coronary stenosis percentage quantification was less accurate than absolute parameters, as seen in a diameter stenosis cutoff that was 61% higher than in other studies.
In another limitation, the results showed moderate correlation with among multiple observers with different experience levels, who also used different postpocessing techniques that enhanced the variation. Other useful parameters for prediction of flow-limiting stenosis include transluminal attenuation gradient downstream of a stenosis, which is helpful for estimating a lesion's functional significant, with an accuracy of about 88% compared with MLA.
CT-based noninvasive fractional flow reserve (CT-FFR) is another promising way to answer the question, although it is burdened by complex postprocessing and only one commercially available software package, they wrote.
Better patient management
Quantitative CTA parameters are useful for patient management in terms of assisting the decision-making process of whether to proceed to ICA or not, the authors concluded. The authors are integrating the techniques into daily practice, and is only quantifying noncalcified or mixed predominantly noncalcified lesions, Feuchtner told AuntMinnieEurope.com.
There is one exception: "Dense calcified lesions may cause too many artifacts such as artificial blooming to be reliable for quantitative analysis," Feuchtner wrote.
The new parameters, combined with the clinical presentation, give cardiologists a fuller picture of what's going on, especially those not specifically trained in reading CCTA, which is still rare in Europe, she said.
"It helps them in decision-making whether to proceed to invasive coronary angiography or stress testing," Feuchtner wrote. The new measures are especially useful in borderline cases when determining whether a lesion is actually closer to 50% or 70% stenosis.