MRI is accurate for detecting problems in children with lower airway tract infection and can pinpoint the dynamics of morphologic changes during treatment, and soon it may replace CT in cases of complicated pneumonia, according to award-winning German research.
In cases of lower airway tract infection, chest x-ray typically is the initial imaging modality. During a prolonged clinical course, repeated chest x-ray or CT exams are often required for management of complications, thus increasing radiation exposure. Cross-sectional imaging can be of significant benefit in children with severe pneumonia, so now there is a strong need for a radiation-free imaging modality that accurately detects complications and precisely evaluates therapeutic management, noted Dr. Jan Müller, from the department of diagnostic and interventional radiology at the University of Heidelberg.
"MRI has been shown to be superior in detecting abscess formation in lower airway tract infection," Müller explained. "Using a modified morphological scoring system, MRI is more sensitive in detecting typical morphologic criteria of airway infection and more accurate in evaluating response to therapy compared with chest x-ray. Thus, employing serial MRI for evaluation of children with complicated lower airway tract infection may lead to significant changes in clinical and therapeutic management decisions without the need of radiation exposure."
Cum laude award at ESTI 2015
The Heidelberg researchers presented their experiences of the complications of pediatric lower airway tract infection in an e-poster at the 2015 annual meeting of the European Society of Thoracic Imaging (ESTI), held in Barcelona, Spain. The ESTI judges gave them a prestigious cum laude award for their work in this area.
The aim of their retrospective study was to evaluate the potential of lung MRI compared with chest x-ray in detecting complications and typical morphological parameters of lower airway tract infections at different time points during treatment.
Müller et al conducted synchronous (interval 1.7 ± 1.5 days) chest x-ray and 1.5-tesla MRI examinations of 21 pediatric patients (age 4.8 ± 3.8 years) after initial calculated therapy of confirmed lower airway tract infection with persistent clinical and laboratory signs of infection. Imaging was repeated after an interval of 17 ± 16.8 days in 11 patients.
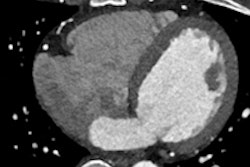
All exams were independently reviewed for the presence of abscess/necrosis, bronchial wall thickening/bronchiectasis, mucoid impaction, and pleural effusion/reaction by a blinded reader. Using a previously evaluated modified morphological scoring system, findings were rated for each lobe (MRI) or lung-field (chest x-ray) depending on the percent size of the area affected: 0 (no abnormality), 1 (< 50% of the lobe involved), or 2 (50% or more of the lobe involved). Subscores for each imaging parameter were calculated for chest x-ray and MRI, and the sum of the subscores resulted in a global score for both imaging modalities.
Key results revealed
Significantly more pulmonary abscesses/necroses (n = 16) were noted in MRI compared with chest x-ray (n = 8) (p < 0.01). MRI described bronchial-wall thickening/bronchiectasis for n = 18 versus chest x-ray with n = 8 (p < 0.01). The global score as well as the subscores for all imaging parameters were significantly higher in MRI compared with chest x-ray (p < 0.01) (Table 1).
| N = 21 | X-ray | MRI | P-value |
| Abscess/necrosis | 13 | 33 | < 0. 01 |
| Bronchial wall thickening/bronchiectasis | 15 | 85 | < 0.001 |
| Mucoid impaction | 1 | 20 | < 0.01 |
| Pleural effusion/reaction | 62 | 106 | < 0.01 |
| Global score | 91 | 244 | < 0.001 |
For the 11 patients undergoing repeated exams, MRI detected more abscesses (n = 9/n = 7) compared with chest x-ray (n = 5/n = 4) at both imaging time points.
Similarly, MRI scored significantly higher for pleural effusion/reaction (p < 0.01) and mucoid impaction (p < 0.05) at first and for abscesses (p < 0.05) and bronchial wall thickening/bronchiectasis (p#0.01) at both imaging time points. On MRI, the global score and the subscores for abscess/necrosis and pleural effusion/reaction significantly (p < 0.05) improved between the two time points during therapy, whereas on chest x-ray, no significant differences were noted (Tables 2 and 3).
| Chest x-ray (n = 11) | Time point 1 | Time point 2 | P-value |
| Abscess/necrosis | 9 | 4 | > 0. 05 |
| Bronchial wall thickening/bronchiectasis | 11 | 16 | > 0.05 |
| Mucoid impaction | 1 | 1 | > 0.05 |
| Pleural effusion/reaction | 32 | 30 | > 0.05 |
| Global score | 53 | 51 | > 0.05 |
| MRI (n = 11) | Time point 1 | Time point 2 | P-value |
| Abscess/necrosis | 19 | 14 | 0.025 |
| Bronchial wall thickening/bronchiectasis | 54 | 18 | > 0.05 |
| Mucoid impaction | 13 | 5 | > 0.05 |
| Pleural effusion/reaction | 62 | 41 | 0.023 |
| Global score | 148 | 108 | 0.032 |
The authors conceded, however, their study was limited by the time interval between chest x-ray and MRI studies, which may reduce comparability because of dynamics in the appearance of morphological findings and interim therapeutic interventions.
Müller was assisted by colleagues from the Translational Lung Research Center Heidelberg (TLRC), Thoraxklinik at University of Heidelberg, and the department of translational pulmonology and Division of Pediatric Pulmonology and Allergy and Cystic Fibrosis Center at University of Heidelberg.