Breast MRI can reliably exclude malignancy when it's applied as a problem-solving tool, and breast imaging guidelines should be adjusted accordingly, say researchers from the Medical University of Vienna.
"We know MR has a high sensitivity for detection of breast cancer, but, interestingly, there's no consensus of the use of MRI to problem solve," according to Dr. Pascal Baltzer from the department of radiology at the Medical University of Vienna.
 Right now there's no consensus on whether breast MRI is a problem-solving tool, said Dr. Pascal Baltzer from the department of radiology at the Medical University of Vienna.
Right now there's no consensus on whether breast MRI is a problem-solving tool, said Dr. Pascal Baltzer from the department of radiology at the Medical University of Vienna.
In 2008, a study by the Society of Breast Imaging in European Radiology found breast MRI could be used as a problem-solving tool when conventional imaging findings are inconclusive (July 2008, Vol. 18:7, pp. 1307-1318). However, in 2010, the European Society of Breast Cancer Specialists (EUSOMA) concluded there was no evidence in favor of breast MRI as a diagnostic tool to characterize equivocal findings at conventional imaging when needle-biopsy procedures can be performed (European Journal of Cancer, May 2010, Vol. 46:8, pp. 1296-1316).
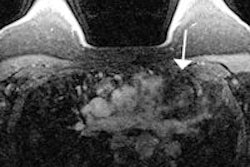
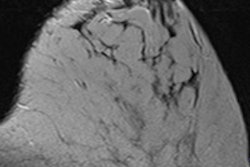
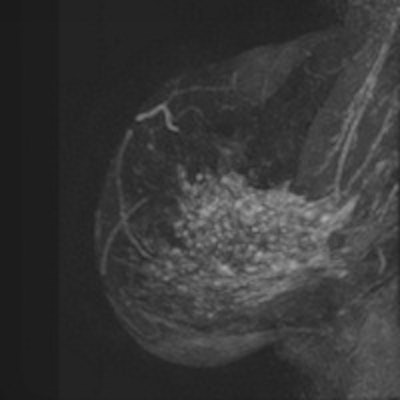
If breast MRI were to be used as a problem-solving tool, it would follow inconclusive mammographic or sonographic findings. If breast MRI were not used, the patient would be biopsied, have additional exams, and experience short-interval follow-ups.
Baltzer and his colleague, Dr. Barbara Bennani-Baiti, sought to effectively evaluate breast MRI as a problem-solving tool and provide solid data for future guidelines. The problem with previous meta-analyses has been selection criteria, Baltzer told delegates at ECR 2014.
The researchers performed a systematic review of PubMed using predefined search terms. They selected only studies in which breast MRI was used for problem-solving purposes such as inconclusive mammographic or sonographic findings. The reference standard had to be established either by histopathology or follow-up exams.
In addition, study design, technical parameters, and the numbers of true positives, false positives, false negatives, and true negatives were extracted from the original publications, and possible bias was determined using the QUADAS 2 applet. Statistical analysis included data pooling, forest plot construction, and heterogeneity testing.
Eleven studies met the inclusion criteria and constituted 1,062 lesions, including 777 benign and 285 malignant lesions. The negative predictive value (NPV) ranged from 87.5% to 100%, with a pooled NPV of 99.1%. The positive predictive value (PPV) was highly heterogeneous (p < 0.0001) ranging from 25% to 96.4%. Based on a random effects model, the pooled PPV was 53.2%.
Post-test probabilities
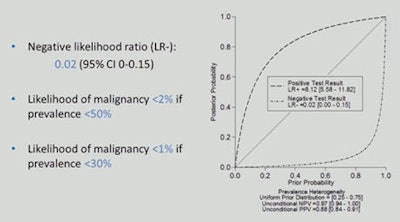 Post-test probabilities show the respective likelihoods of malignancy. Source: Dr. Pascal Baltzer.
Post-test probabilities show the respective likelihoods of malignancy. Source: Dr. Pascal Baltzer."Can MRI exclude malignancy? Yes it can," Baltzer said. "Breast MRI reliably excludes malignancy when conventional imaging is inconclusive. We strongly recommend its use as a problem-solving tool."
In fact, in their daily clinical practice, the researchers are already using MRI in this way. Their main indications in terms of numbers are preoperative staging, problem solving, and high-risk screening, Baltzer stated in an email interview with AuntMinnieEurope.com.
In Austria, problem solving is a very common indication used for breast MRI, which also receives insurance reimbursement.
"This is not so in Germany," he said. "The restrictive use of breast MRI in this neighboring country underlines the need for evidence-based recommendations for breast MRI. I hope, after having published our full paper, future guidelines will clearly acknowledge the value of breast MRI as a problem-solving tool in noncalcified lesions."
He and his colleagues are planning future studies on breast MRI, particularly its possible use in the management of microcalcifications and its cost-effectiveness as a problem-solving tool, something they have just started to explore.