Assessing the entire field-of-view carefully for abnormalities on breast MRI studies is vital, because some incidental extramammary findings are malignant, and this alters diagnostic workup, staging, and treatment, Croatian researchers have found.
Breast MRI field-of-view evaluates not only the breast and axillae, but includes part of the thorax and upper abdomen. Therefore, examinations can detect findings that are incidental to the initial indication.
"The detection and characterization of these extramammary findings represents a challenge to the interpreting physician, both in terms of assigning clinical significance and determining the appropriate workup for a given abnormality," noted Dr. Ana Marija Alduk from the clinical department for diagnostic and interventional radiology at the University Hospital Centre Zagreb.
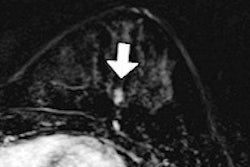
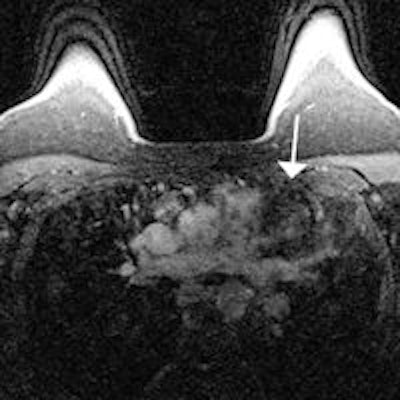
The best way for radiologists to ensure detection of any extramammary findings is to carefully assess all structures within the field-of-view on a turbo inversion-recovery with magnitude display (TIRM) sequence, she emphasized in an interview with AuntMinnieEurope.com.
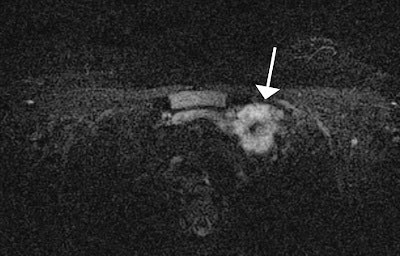
"If any abnormalities are found, I recommend correlating it with contrast-enhanced images," she said. "These images turned out to be most useful for the detection and characterization of extramammary lesions."
Alduk and colleagues defined incidental findings as unexpected lesions outside the breast, not previously known or suspected at the time of referral. They included 500 consecutive breast MRI studies performed from June 2010 to September 2012 in their retrospective study (Clinical Radiology, May 2015, Vol. 70:5, pp. 523-527).
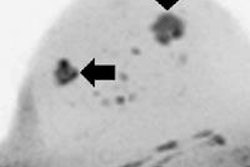
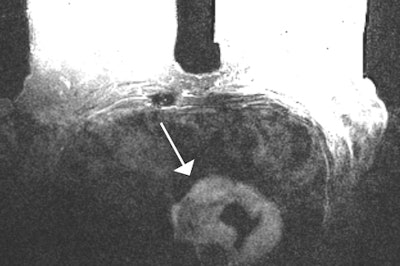
The MRI findings were compared with subsequent diagnostic procedures to differentiate malignant from benign lesions. The researchers detected 138 incidental findings in 107 of the 500 (21.4%) patients. The most common site was the liver (44.2%), followed by the lung (17.4%), mediastinum (15.9%), pleural cavity (10.9%), bone tissue (6.5%), spleen (2.2%), major pectoral muscle (2.2%), and kidney (0.7%).
Of the incidental findings, 18.1% were confirmed to be malignant. Malignant findings were exclusively detected in patients with known breast carcinoma, whereas incidental findings in patients without a history of carcinoma were all benign, according to Alduk and colleagues. Also, 24.8% of incidental findings among patients with history of breast cancer were malignant.
"Few studies are published concerning the prevalence and nature of incidental extramammary findings at breast MRI," they stated. "The present study confirms that breast MRI may reveal a large number of incidental extramammary findings. It is consistent with previous studies in terms of frequency, distribution, and nature of incidental extramammary findings."
Even though most of the extramammary findings were benign, some were metastatic and required the use of systemic therapy.
"Malignant lesions were exclusively detected in patients with previously known breast carcinoma, which emphasizes the importance of careful assessment of incidental findings in this group," the researchers added. "The present study showed that the prevalence of malignant findings in patients with a history of breast cancer is dependent on location, with the high likelihood of bone lesions being malignant (100%) in comparison to other locations."
Bone lesions are more likely to be malignant in comparison with other locations, probably because of the wide spectrum of benign abnormalities encountered in the liver (cysts and hemangiomas) or pleural cavity (effusions). Thus, a new bone lesion in a patient with breast carcinoma should be considered malignant until proved otherwise and should prompt further diagnostic workup. Also, 11.6% of hepatic lesions were metastatic, altering further treatment, so indeterminate lesions that do not satisfy the criteria for cysts or hemangiomas require further diagnostic workup (using ultrasound, CT, or liver MRI).
Among patients with preoperative breast MRI, none had lung metastases, although they can be found in 5% to 10% of breast cancer patients at presentation, changing the treatment plan. This is probably due to a limited role of breast MRI in the evaluation of lung nodules because of its limited spatial resolution compared with multidetector CT, high susceptibility differences between airspaces and the pulmonary parenchyma, and the presence of respiratory and cardiac motion, the authors wrote.
"Most of small pulmonary nodules are benign, but metastases, bronchogenic carcinoma, and other malignant causes must be excluded," they added. "Pulmonary nodules < 4 mm in low-risk patients without a history of cancer do not require follow-up. Additional CT is indicated for patients known to have or suspected of having malignant disease, as well as in cases of larger pulmonary nodules."
The main limitation of the study is its retrospective nature, so the exact influence on follow-up, staging, and treatment can't be determined, although an effect can be expected considering the large number of malignant findings detected., the authors wrote. To counter this, Alduk and colleagues are planning a prospective study that would determine exact clinical impact of incidental extramammary findings -- their influence on follow-up, staging, and treatment.
"As a result of this study, radiologists interpreting breast MRI in our institution are more aware of the possibility and potential clinical impact of extramammary findings," she said. "It seems to me that the number of reported extramammary findings increased significantly since the study."