For cryoablation to be more widely accepted in breast cancer therapy, there must be paradigm shifts in how the medical community looks at treatment options and their outcomes, Prof. Dr. Michael Fuchsjäger, head of radiology at the Medical University of Graz in Austria, told Arab Health attendees.
Minimally invasive cryoablation can be used effectively to treat breast cancer without the need for general anesthesia, Fuchsjäger explained in a talk given on 25 January at the Total Radiology Conference at Arab Health 2022 in Dubai. However, the procedure should be used for small unifocal lesions, and not for larger multifocal multicentric tumors, as well as invasive lobular breast cancer and ductal carcinoma in situ.
 Prof. Dr. Michael Fuchsjäger. Images courtesy of Robert Stevens.
Prof. Dr. Michael Fuchsjäger. Images courtesy of Robert Stevens.Fuchsjäger, who is chairman of the ESR Board of Directors, highlighted the multiple advantages of providing minimally invasive methods to kill tumor cells in women through ablation, as opposed to conventional surgeries. This is particularly important at present, given the urgent need to reduce overtreatment of certain tumor types.
He pointed to how he worked on just one minimally invasive operation in 2021. "I would love to do 100, because it's an easy procedure for an experienced radiologist with ultrasound guidance," he said.
Tumor ablation has been explored in recent years as a minimally invasive way to treat solid cancers through chemical or thermal therapies, with more success seen in smaller tumors.
"If you correctly use minimally invasive therapy, you don't need general anesthesia," he continued. "All these procedures can be performed on an outpatient basis. The cosmetic outcome is definitely better if we use a one-millimeter needle instead of a surgical incision."
The advantages of this approach include reduction of time and cost, as well as improvements in overall patient outcome and experience.
Optimum use of imaging
Ultrasound, MRI, mammography, and CT have all been used to guide and position needle probes. The probes are attached to a generator, and once a probe is inserted into the tumor, it kills cancer cells by burning the tumor at above 50°C or freezing the tumor below -40°C .
While most minimally invasive therapies don't require anesthesia, conscious sedation can be used to relax patients and ease pain.
Thermoablation, where extreme heat is used, requires probes with needle sizes ranging from 1.6 mm to 2 mm. The heat generator can be radiofrequency, microwave, or focused ultrasound.
Fuchsjäger said ultrasound guidance can be considered noninvasive in this scenario, even though the procedure can be "tricky" and is operator-dependent and takes "a lot of time" when using cryotherapy.
With cryoablation, thinner needles are used, between 1.2 mm and 2 mm. Argon gas or liquid nitrogen are used, and imaging modalities are used to guide needle electrode placement (ultrasound, mammography, MRI). The surrounding skin is meanwhile continuously warmed, and several freeze-thaw cycles are employed. The coldness prevents the patient experiencing pain.
What the literature says
Significantly, the U.S. Food and Drug Administration has recognized cryoablation for the treatment of fibroadenoma.
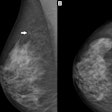
A 2004 study published in Radiology found that cryoablation achieved complete necrosis for tumors in seven out of nine invasive ductal carcinoma cases. The tumors were less than or equal to 1.8 cm wide. The researchers used two freeze-thaw cycles ranging from 32 to 40 minutes each.
Another study published in 2011 in European Radiology found that 14 out of 15 tumor cases achieved complete necrosis. One needle electrode was used, and two freeze-thaw cycles were used here as well.
 Fuchsjäger worked in the Middle East from 2009 to 2012, building up the radiology department at Al Ain Hospital in Abu Dhabi. He has lived in Graz with his wife and five children since 2012.
Fuchsjäger worked in the Middle East from 2009 to 2012, building up the radiology department at Al Ain Hospital in Abu Dhabi. He has lived in Graz with his wife and five children since 2012."These first studies actually show that minimally invasive therapy with freezing is feasible. It was successful in the treatment of early-stage breast cancer," Fuchsjäger said. "Our friends from surgery say it's easy to excise small cancers with local anesthesia, but percutaneous treatment is the approach of the future -- at least for some types of disease."
He emphasized the benefit that patients experience no pain throughout the procedure.
But some requirements must be met to consider either method. Tumors must be less than or equal to 2 cm wide and be visible on the imaging modality chosen to guide the treatment. The distance from the tumor to the skin and the pectoral muscle must also be greater than or equal to 1 cm to avoid damage to the nearby structures.
Fuchsjäger's academic and clinical interest is primarily focused on breast radiology and intervention, including minimally invasive therapy as well as assessment of 4D blood flow and tissue characterization by cardiac MRI. His time focusing on Arab health has been recognized over the years. Between 2009 and 2012, he helped rebuild and expand a small and aging radiology unit in the United Arab Emirates to include digital imaging.
The unit's efforts were acknowledged in 2010 with accreditation from the Joint Commission International (JCI), as well as an Excellence in Digital Imaging and Diagnostics award received in 2012 from the Arab Health congress.
Editor's Note: Our editorial advisory board member Dr. Elisabetta Giannotti carried out a technical edit of this article.