Deep learning applied to liver MRI scan data can predict the development of cardiovascular disease, German researchers have shown.
In a study published online by JHEP Reports on 22 April, Dr. Jakob Nikolas Kather from the Medical Oncology Department of the National Center for Tumor Diseases at University Hospital Heidelberg and colleagues investigated the application of transformer neural networks using liver MRI data from the U.K. Biobank’s collection to determine their efficacy in cardiovascular risk prediction.
Cardiovascular disease is often associated with underlying metabolic disorders, the authors wrote. The liver, as the primary metabolic organ, could be used as an indicator of the metabolic changes that are precursors to cardiovascular disease, and major adverse cardiac events (MACEs) in particular. Establishing imaging-based, noninvasive biomarker testing for cardiovascular risk assessment in patients (especially those not yet manifesting signs of disease) would enable earlier diagnosis, but it has proven challenging.
“On a practical level, we strive to develop an enhanced biomarker that efficiently incorporates quantitative information about metabolic risk factors, paving the way for more personalized and targeted prevention strategies,” the researchers stated.
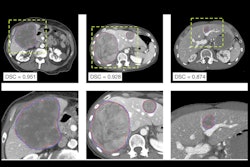
The team used transformer neural networks, a newer, more flexible type of neural network, to develop a liver-MRI foundation model trained through self-supervised learning on 44,672 U.K. Biobank single-slice liver MRIs.
Of these scans, those used for the training included a combination of all of those with a recorded occurrence of MACE before the liver MRI exam (974), along with the majority of participants with no history of MACE before the MRI (43,698). An additional 750 (all 214 participants with first-time MACE after the MRI, and 536 randomly selected participants with no history of MACE both before and after the MRI) were used for external validation. In all, there were 45,422 participants.
The researchers assessed the predictive ability of the model by comparing predicted risk scores with the actual cardiovascular outcomes.
In addition, the model’s risk scores were compared with those generated by SCORE2. The team then evaluated the results of subgroups based on identified risk factors from SCORE2 (e.g., diabetes, cholesterol, systolic blood pressure, sex, and smoking status) within our model’s prediction scores to “provide insight into which cardiovascular risk factors are being captured in a more pronounced way by our model.”
The results showed that the model has “significant discriminatory capacity” for predicting MACE and cardiovascular-related mortality, even outperforming methods such as SCORE2, the authors said.
However, they noted that, even with the model showing promising utility as an imaging-based biomarker for assessing cardiovascular risk, the use of MRI as a widespread screening tool would be impractical, given its high cost and challenges with accessibility. Rather, they suggested that it would be most appropriate for high-risk groups, or in scenarios where data is already available (e.g., patients known to have underlying metabolic disorders, or those with liver imaging performed for other reasons).
The study's retrospective scope and restriction to single-slice liver imaging might have introduced bias, the authors wrote. Also, the authors noted a lack of detailed liver metrics (such as those that might have indicated mild liver disease). They suggested that future studies should incorporate additional clinical and imaging data for enhanced predictive accuracy, and any future studies should include a completely independent external validation cohort.
Kather and colleagues concluded that their study showed that such models, once refined, could be incorporated into clinical practice.
Read the study here.