
More than a third of radiology departments are using AI in clinical practice, particularly for lung-nodule detection on CT, stroke diagnosis, and bone age prediction, a survey conducted in the Netherlands has found.
Most respondents experienced added value in terms of decreased costs and/or improved outcomes from using AI-based software, but the major obstacles to adoption remain the costs and IT-related difficulties, lead author Kicky van Leeuwen and colleagues from Radboud University Medical Center in Nijmegen noted in an article posted by European Radiology on 29 July.
The authors' goal was to map the clinical use of CE-marked AI-based software in radiology departments in the Netherlands (n = 69) between 2020 and 2022. They sent a questionnaire each spring from 2020 to 2022 about AI product usage, financing, and obstacles to adoption. Products not listed on www.AIforRadiology.com by July 2022 were excluded from the analysis.
The number of respondents was 43 in 2020, 36 in 2021, and 33 in 2022, according to the researchers. The number of departments using AI grew steadily from 14 in 2020 to 19 in 2021, and 23 in 2022.
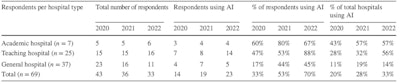 Use of AI per hospital type as reported by the respondents. All figures courtesy of Kicky van Leeuwen et al and European Radiology.
Use of AI per hospital type as reported by the respondents. All figures courtesy of Kicky van Leeuwen et al and European Radiology.The diversity of products implemented increased by fivefold from seven unique products in 2020 to 34 in 2022. The cumulative number of AI implementations was 19 in 2020, 38 in 2021, and 68 in 2022.
"Departments using AI had on average one AI product running in 2020, two in 2021, and three in 2022," the group noted. "In 2022, six departments were reported to have discontinued the use of in total seven products. Four hospital organizations said to use an AI platform or marketplace for the deployment of AI solutions."
In 2022, AI was mostly used to support chest CT analysis (nodule detection, pulmonary embolism detection, COVID severity; n = 17), neuro CT analysis (large vessel occlusion detection, intracranial hemorrhage detection, ASPECTS, CTP; n = 17), followed by musculoskeletal radiograph analysis (bone age prediction, fracture detection, and automated extremity measurements; n = 12).
According to the authors, "From all respondents that used AI clinically in their department, 28% stated that the implemented AI products realized health improvement and 32% assumed both health improvement and cost savings. No one reported cost savings alone. Value was considered unclear for 32% of the respondents and 8% said to experience no added value."
Barriers to implementation
The most important obstacles to the adoption of AI remained costs and IT integration.
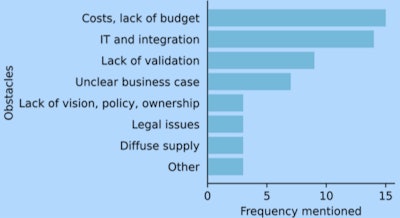 Main obstacles experienced for the purchase, validation, and implementation of AI tools in clinical practice as responded in 2022. Bars represent the frequency of the item mentioned by respondents. Multiple items per respondent were possible.
Main obstacles experienced for the purchase, validation, and implementation of AI tools in clinical practice as responded in 2022. Bars represent the frequency of the item mentioned by respondents. Multiple items per respondent were possible.In both 2021 and 2022, 13 respondents mentioned that their center had a budget reserved for radiology AI purchases in the coming year (36% in 2021, 39% in 2022). The remainder had no budget or did not know whether there was a budget reserved. Financial resources originate from the institutional level, the radiology department, or both. The source slightly shifted to the departmental level in 2022.
The adoption of AI products in radiology departments in the Netherlands is showing common signs of a developing market. The major obstacles to reaching widespread adoption are a lack of financial resources and IT integration difficulties.
"The clinical impact of AI starts with its adoption in daily clinical practice," the authors stated. "Increased transparency around AI products being adopted, implementation obstacles, and impact may inspire increased collaboration and improved decision-making around the implementation and financing of AI products."
You can read the full article on the European Radiology website.



















