An artificial intelligence (AI) algorithm that screens head CT exams for intracranial hemorrhage (ICH) -- and triages suspected cases for radiologist review -- can yield significant improvements in patient outcomes, researchers from Israel reported in a Wednesday presentation at ECR 2021.
After retrospectively reviewing ICH cases for a year before and a year after adoption of a commercial deep-learning algorithm, Dr. Daniel Raskin and colleagues from Sheba Medical Center in Tel Aviv found that the use of AI led to decreased patient mortality, readmission rates, and disability.
"Such AI technology may help prioritize radiology workflow, decrease the time lag between scan and diagnosis, and result in favorable patient outcomes," said Raskin, a radiology resident.
Although the number of diagnostic imaging exams and the number of images per scan continues to increase, the number of radiologists remains pretty much the same. And radiologists still largely work based on the same method: first study in, first study out, according to Raskin.
Patient outcomes depend greatly on an accurate and timely diagnosis, however. That creates the need for AI-based worklist prioritization in radiology, he said.
Sheba Medical Center has served as an alpha site for AI software developer Aidoc since 2016, and completed real-time, real-world integration of the vendor's deep learning-based software for acute CT exams in June 2018.
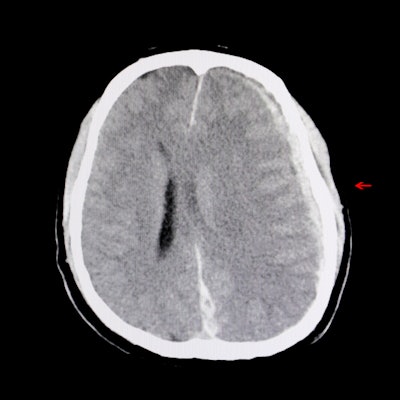
The software analyzes every head CT study after acquisition. If an abnormality is detected, it then triggers a pop-up notification for the radiologist. The suspected abnormality is also highlighted on the image for the radiologist to review, Raskin said.
To assess the impact on patient outcomes of using AI to flag patients with ICH in an emergent care setting, the researchers retrospectively reviewed consecutive noncontrast head CT exams and electronic medical record data from the institution's ED for the presence of pathological intracranial hyperdense lesions. They gathered all cases from 2017 before AI was implemented and then in 2019 after AI was adopted.
The study involved 548 patients, including 299 (46%) from the pre-AI year and 349 (54%) from the post-AI year. No statistically significant differences were found between the two groups of patients for demographics, emergency severity score, type of ICH, complete blood count, comorbidities, and smoking history, according to researchers.
The authors then assessed 30-day and 120-day mortality in these patients for both years and also recorded 120-day readmission rates, Modified Rankin Scales for patient function, and inpatient lengths of stay.
| Outcome measures for ICH patients before and after adoption of AI | ||
| 2017 (Before AI) | 2019 (After AI) | |
| 30-day all-cause mortality | 27.3% | 16.8% |
| 120-day all-cause mortality | 30.8% | 20.5% |
| 120-day readmission rate | 37% | 25% |
| Modified Rankin Scale | 3.17 | 2.84 |
The differences were statistically significant for all-cause mortality rates (p < 0.005), readmission rate (p < 0.005), and Modified Rankin Scale (p = 0.044).
"Implementation of AI software for flagging patients with intracranial hemorrhage for a year resulted in a significant reduction in mortality rate, readmission rate, and Modified Rankin Scale," Raskin said.



















