As the number of patients diagnosed with cancer continues to increase, and the technologies employed to treat such indications evolve, the amount of clinical data being recorded and analyzed is growing at an unprecedented level. "We have information coming at us at a rate that no human could possibly keep up with," said Susan McLaughlin from IBM Watson Health.
 Richard Hausmann, CEO of Elekta.
Richard Hausmann, CEO of Elekta.At the recent ESTRO 37 congress, speaking at a symposium hosted by Swedish radiation oncology vendor Elekta, McLaughlin explained this data onslaught was IBM's motivation for creating Watson for Oncology, an artificial intelligence (AI)-based clinical decision support system. The tool was developed in collaboration with the Memorial Sloan Kettering (MSK) Cancer Center, which provided training by expert clinicians using patient records and published guidelines. This was supplemented with millions of pages of text from over 300 research journals articles and 250 medical textbooks.
Earlier this year, Elekta announced collaboration with IBM to offer Watson for Oncology within its digital cancer care systems, including integration into its widely used Mosaiq oncology information system. "Joining forces with IBM Watson Health positions Elekta as the first radiation therapy company to offer capabilities that combine conventional health information systems with artificial intelligence and cognitive cloud computing," said Richard Hausmann, Elekta's CEO. Medicalphysicsweb editor Tami Freeman spoke to Hausmann to find out more.
Tami Freeman: What was Elekta's motivation for collaborating with IBM Watson Health?
Hausmann: Elekta has two product offerings, firstly the treatment solutions, which are the machines that deliver the dose and the associated software. On top of that is what I call a digitization level of healthcare, our Mosaiq workflow software, which supports all data accumulation and storage of relevant data. Mosaiq manages the patient from diagnosis through the whole therapeutic workup, whether this is radiotherapy, chemotherapy, immunotherapy, or surgery.
Within this digitized world, between diagnosis and treatment, there is typically a tumor board where experts come together to decide on the appropriate treatment for the patient. But in many cases, you don't have all the experts available to do this effectively. Here, it makes sense to have a tool like Watson for Oncology.
So how does Watson for Oncology work with Mosaiq?
Basically, all of the patient's information is input into Watson, both data from Mosaiq and also from the diagnostic side, such as images, diagnoses, lab data -- all the things that a tumor board typically sees. The data from the patient are then mirrored to the closest case at MSK, and Watson finds the most probable treatment that MSK would perform.
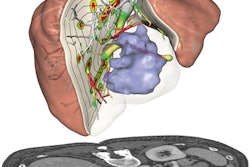
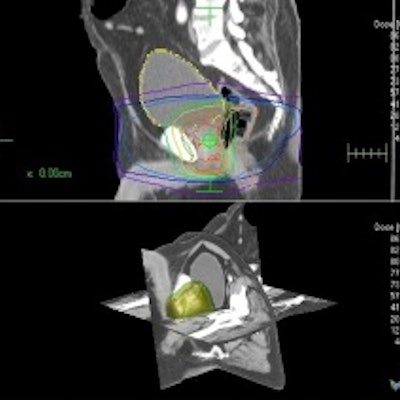
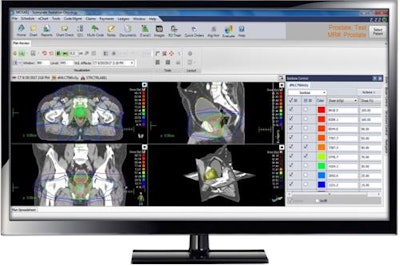 Elekta's digital cancer care and its Mosaiq oncology information system. Credit: Elekta.
Elekta's digital cancer care and its Mosaiq oncology information system. Credit: Elekta.This is where the AI comes in -- Watson also examines all of the studies that are relevant for this particular dataset, and all of the publications in the field. It then creates probabilities of what would be the best therapy to use and provides a treatment recommendation -- such as radiotherapy with a certain number of fractions, chemotherapy, and radiation first to reduce the tumor size and so on.
Where will this technology be of most benefit?
This approach comes into play in situations where not all of the experts are in place, such as in developing countries where there can be a huge lack of oncologists, but still a huge need for treatments. Watson can extend the capabilities and knowledge of the few oncologists that there are, and increase access to care.
It also comes into the game for standardization of treatments in larger hospital chains or cancer centers, where variability of care can be significant. Here, the aim of using Watson is to create reproducible, standardized procedures. We see a huge application there as well.
Watson is really a workflow tool. Instead of having experts in place, you can use the accumulated experience that was put into Watson and correlate this with your patient's dataset. Or you can use Watson as a control, if you have decided how best to treat, but want to check it against what MSK would have done.
 Elekta Mosaiq colleagues and the IBM Watson Health delegation, including (far left) IBM's Susan McLaughlin, at ESTRO 37.
Elekta Mosaiq colleagues and the IBM Watson Health delegation, including (far left) IBM's Susan McLaughlin, at ESTRO 37.Does Elekta plan to use Watson with its Monaco treatment planning system?
This collaboration is just starting -- this is such a big area that we'll do it step by step -- but I'm sure we'll get to the point where treatment planning forms part of it as well. To automate contouring for dose planning and dose calculation, for example, or to find organs-at-risk in images from the MR-linac, then these tools will get more and more important. And with every patient, the system learns -- this is what deeper AI algorithms do. As well as improving quality, it will also make planning faster.
Will this help with adaptive treatments, on the MR-linac for example?
In my view, in 10 years from now, there will be no planning scan at all. A patient will be diagnosed and then at every session on the MR-linac, there will be integrated segmentation, planning, and execution, at a speed as fast as a preplanned treatment today. It will happen, no question. And if you go to the next step, real-time adaption where you track moving parts of the body, then of course you will need the speed and automation of AI behind that.
How do you see the future of AI within oncology?
In Elekta's business, we view AI, or deep learning, as a significant foundation for the future. One application, for example, is for tasks that we have to perform quickly and effectively, such as segmenting sensitive organs and the tumor itself. Automated tools can do this faster and more reproducibly than the human eye. It can be used for simpler things too, such as optimizing linac scheduling in case of unexpected events.
We also see AI as an important tool for improving our own products. Today, we choose which sensors to put into our systems and monitor these constantly. If a parameter changes, we conclude that we should perform preventative maintenance or exchange a part. I call this the "dipstick method" -- you know what to look for, you make a sensor, and you act on some parameters.
With AI, you could imagine a situation where you stream numerous data from a system, even things that you may not think relevant. With such a stream of data coming in, you can constantly evaluate correlations between those parameters and the status of the system. This would enable you to prepare to take action without even needing to know the actual physical correlation.
This seems to be a really interesting approach for preventative remote service. And because all our systems around the world are connected with our server, that is something that in principle can be implemented pretty soon.
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.