
Integrating medical students into the radiology reading room can have major long-term benefits, and the accuracy of medical students' reports is only slightly inferior to that of first-year residents, Swiss researchers have reported at the virtual RSNA 2020 meeting.
 Dr. Jan Vosshenrich of University Hospital Basel.
Dr. Jan Vosshenrich of University Hospital Basel."Active integration of medical students fosters their understanding and interest in our field. Potential candidates for residency can be identified among them," noted lead author Dr. Jan Vosshenrich, a radiologist at University Hospital Basel in Switzerland. "Structured reporting seems to be beneficial for radiology beginners."
The current learning practice of medical students in radiology is mainly observational, and students tend to shadow radiologists in the reading room rather than participating actively in the reporting process, Vosshenrich and colleagues explained in a digital poster. Only a few studies have investigated the close involvement of medical students, and they mainly comprise using virtual radiology workstations.
"There is thus a need for active engagement of medical students during their elective rotations," they stated.
How they do it in Basel
During the past three years, the Basel group's main goal has been to assess the performance of final-year medical students when they are integrated into radiology workflow during their elective rotation rather than passively observing. Medical students' work is reviewed with an attending radiologist, and reports are then corrected and sent for sign-off. A similar workflow exists for radiology residents.
Each month up to four medical students perform an elective rotation in the radiology department. Students receive a RIS/PACS training session on their first day to familiarize themselves with the software and workflow. Students spend one week in each of the four core subspecialty sections: body imaging, cardiothoracic imaging, musculoskeletal imaging, and neuroradiology. They can choose selected imaging studies (nonacute outpatient examinations) from the respective worklists and dictate draft reports.
Vosshenrich and colleagues used an anonymized database extract to assess the performance of medical students. Reports dictated between October 2017 and March 2020 were included in the analysis. The authors compared the mean report similarity between the two reporting standards: structured reporting versus free-text reporting. They also compared the students' performance with that of first-year residents.
A total of 8,120 reports dictated by 92 medical students were analyzed (mean, 88.3 reports).
Of these reports, 6,711 were for radiography, 848 were for CT, and 561 were for MRI. Body imaging accounted for 467 reports, cardiothoracic imaging 3,659, musculoskeletal imaging 3,143, and neuroradiology 854.
The mean similarity of reports dictated by medical students was higher in subspecialty sections using structured reporting compared with divisions relying on free-text reports. The mean was 0.63 versus 0.47 (p < 0.001). No differences in similarity were observed between imaging modalities (range, 0.50-0.56).
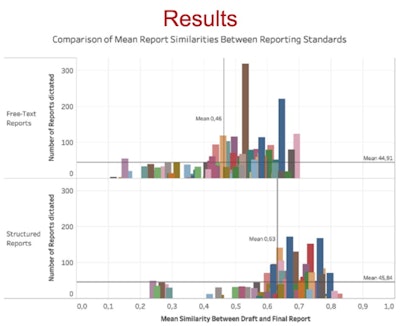 Bar charts comparing mean report similarities between reporting standards. Each bar represents one distinct medical student. Figure courtesy of RSNA 2020 and Dr. Jan Vosshenrich.
Bar charts comparing mean report similarities between reporting standards. Each bar represents one distinct medical student. Figure courtesy of RSNA 2020 and Dr. Jan Vosshenrich.Thirteen first-year residents started their residency in the radiology department from October 2017 and March 2020. Within the first month, they dictated an average of 185.5 reports (97.2 more than medical students). The mean report similarity was slightly higher compared with the medical students. The mean was 0.61 versus 0.55 (p < 0.001).
A limitation of the study was its single-center retrospective analysis. Also, the study may not be reproducible in other regions due to billing reasons and because medical students are not allowed to dictate reports of "real" patients in some countries, the authors explained. Finally, only quantitative assessment was involved, and the Jaccard similarity coefficient does not provide information on the significance of edits, they concluded.



















