Pediatric lung MRI holds great potential as a radiation-free alternative to CT, offering superior soft-tissue contrast and functional imaging capabilities, according to award-winning research. Continued technological advances in MRI may further enhance its role in the comprehensive assessment of pediatric thoracic diseases.
Thoracic MRI has become viable for many pathologies, offering high sensitivity and specificity in several conditions. The indications can be broadly divided into lung parenchymal, mediastinal, and chest wall pathologies, with its diagnostic utility being particularly significant in children due to its radiation-free nature.
“MRI demonstrates high sensitivity for detecting pneumonia, its complications (e.g., necrosis, abscess), and other lung abnormalities,” noted Dr. Emre Ruhat Avci and his colleagues from the Department of Radiology at Dokuz Eylül University Faculty of Medicine, Izmir, Turkey. “It also aids in narrowing differential diagnoses by identifying specific features such as necrosis and cavitation in tuberculosis or the characteristic hydatid cysts in Echinococcus infections.”
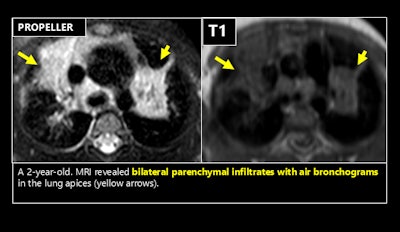 Techniques such as undersampling k-space or employing specialized k-space sampling strategies, including periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER or BLADE), are effective in minimizing respiratory motion artifacts and improving image quality in challenging cases. Figures courtesy of Dr. Emre Ruhat Avci et al and presented at ECR 2025.
Techniques such as undersampling k-space or employing specialized k-space sampling strategies, including periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER or BLADE), are effective in minimizing respiratory motion artifacts and improving image quality in challenging cases. Figures courtesy of Dr. Emre Ruhat Avci et al and presented at ECR 2025.
In cystic fibrosis, MRI can detect active inflammation through bronchial wall enhancement and distinguishes mucus plugs from thickened walls, and it can be used to assess lung perfusion changes due to hypoxic vasoconstriction or tissue damage, with perfusion alterations, they explained in an ECR 2025 poster that received a cum laude award.
“Historically limited by challenges such as low lung proton density and air-tissue interface, advancements in MRI technology have significantly enhanced its utility,” they commented. “MRI is now sensitive for detecting and characterizing solid lung lesions, infiltrative disorders, respiratory mechanics, ventilation, perfusion, and mediastinal pathologies.”
MRI is proving useful for congenital anomalies and malformations, including pulmonary sequestration, congenital pulmonary airway malformation, congenital diaphragmatic hernia, and congenital lobar emphysema. For interstitial lung diseases, MRI has limited utility compared to CT due to lower signal resolution, but recent studies suggest it may be useful in differentiating between areas of active inflammation and fibrosis, the researchers stated.
Additionally, MRI can be effective for evaluating large airway pathologies, including masses and structural abnormalities, and for assessing pulmonary involvement in systemic conditions such as vasculitis, connective tissue diseases, and hematological disorders. The modality effectively demonstrates nodular and cavitary lesions in the lung parenchyma, they pointed out.
MRI has a high sensitivity for mediastinal lymphadenopathy, too, and it is comparable to CT in diagnosing mediastinal masses and cystic lesions, and the technique effectively visualizes lesion contents, such as fat, distinguishes vascular structures, and assesses pericardial and chest wall invasion.
 Dr. Emre Ruhat Avci with his co-author and mentor Dr. Ceren Sarioğlu, an associate professor of radiology at Dokuz Eylül University.
Dr. Emre Ruhat Avci with his co-author and mentor Dr. Ceren Sarioğlu, an associate professor of radiology at Dokuz Eylül University.
“MRI is effective in detecting embolism in larger pulmonary arteries, thoracic aorta anomalies, anomalous pulmonary venous return, pulmonary artery aneurysms, arteriovenous malformations, and vasculitis,” Avci and colleagues continued. “Advanced MRI angiography techniques enable the acquisition of both arterial and venous phase images with a single contrast injection.”
MRI is excellent too for assessing chest wall tumors and their invasion, and it provides a detailed evaluation of lesion contours and components, such as septations, T2 hypointense fibrous components, and hypointense foci associated with phleboliths.
Overall, it is important to understand the role of lung MRI and indications in pediatric patients, learn the MRI sequences commonly used in lung imaging, and identify the limitations of lung MRI and apply artifact-reducing techniques to improve image quality, the Izmir team emphasized.
To find out more about the equipment, technique, and protocols used by the group and to view more clinical images, you can read the full ECR poster here. The co-authors of the exhibit were Furkan Uncuoğlu, Fatma Ceren Ceren Sarioğlu, and Handan Güleryüz.





















