Awareness of Crohn's disease is growing, but radiologists must also be familiar with lesser known diseases affecting the small bowel because they can be detected in patients referred for small bowel MR enterography or enteroclysis, according to an experienced team of researchers from Amsterdam.
"There are many diseases that may cause similar clinical symptoms or radiological signs to those in Crohn's disease," noted Dr. Giedre Kavaliauskiene, from the department of radiology at Amsterdam's Academic Medical Center, at which more than 2,000 MRI examinations of the small bowel have been performed. "Furthermore, MR enterography and enteroclysis play an increasing role in the detection of other small bowel diseases, including tumors."
 A 37-year-old female patient presented with chronic abdominal pain and was suspected of having irritable bowel syndrome. MR enteroclysis coronal fat-saturated true-FISP image demonstrates the duodenojejunal junction and proximal jejunum loops located on the right-hand side of the abdomen (arrowhead) and the normal position of the ascending colon (AC) and descending colon (DC). All images courtesy of Dr. Giedre Kavaliauskiene.
A 37-year-old female patient presented with chronic abdominal pain and was suspected of having irritable bowel syndrome. MR enteroclysis coronal fat-saturated true-FISP image demonstrates the duodenojejunal junction and proximal jejunum loops located on the right-hand side of the abdomen (arrowhead) and the normal position of the ascending colon (AC) and descending colon (DC). All images courtesy of Dr. Giedre Kavaliauskiene.There seems to be no major differences in accuracy between ultrasound, CT, scintigraphy and MRI in diagnosing inflammatory bowel disease, so it is wise to use a noninvasive technique without radiation exposure to detect small bowel lesions in patients with Crohn's disease, wrote Kavaliauskiene in an article published online on 13 July by Insights into Imaging. Important advantages of MRI are the unrestricted overview, easy comparison between examinations, and improved communication of results to the referring physician. Therefore, MRI is the technique of choice in many centers.
Among the bowel and mesenteric diseases to be aware of are internal hernia, intussusception, neuroendocrine tumor, and familial Mediterranean fever, all of which can mislead radiologists to erroneously diagnose active Crohn's disease, Kavaliauskiene stated. Often, knowledge of findings in these diseases can be sparse.
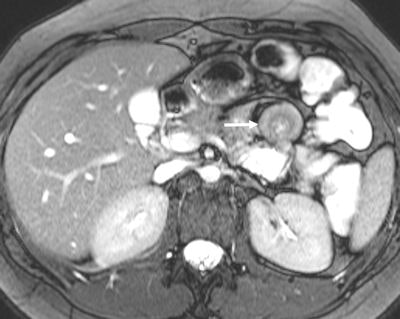
 An 18-year-old female patient complained of abdominal pain, and Crohn's disease was suspected. Top: MR enterography axial fat-saturated true-FISP image demonstrates a target-like small bowel appearance of a small bowel intussusception in the left upper quadrant (white arrow). Bottom: Axial fat-saturated VIBE image after intravenous contrast medium acquired 6 min later at the same level shows no evidence of intussusception. A diagnosis of a transient small bowel intussusception was made. No evidence of Crohn's disease..
An 18-year-old female patient complained of abdominal pain, and Crohn's disease was suspected. Top: MR enterography axial fat-saturated true-FISP image demonstrates a target-like small bowel appearance of a small bowel intussusception in the left upper quadrant (white arrow). Bottom: Axial fat-saturated VIBE image after intravenous contrast medium acquired 6 min later at the same level shows no evidence of intussusception. A diagnosis of a transient small bowel intussusception was made. No evidence of Crohn's disease..Adequate luminal distension is vital to accurately assess the small bowel, and three groups of contrast agents can be used to achieve distension: positive, negative, and biphasic agents. Positive oral contrast agents appear hyperintense on all sequences, and are based on gadolinium-chelate, ferrous, or manganese ions. The high signal intensity of the lumen can interfere with the high signal intensity of the bowel wall after intravenous contrast medium administration. Negative oral contrast agents are based on iron oxide particles. They appear as hypointense on all sequences.
Biphasic oral contrast agents are the most frequently used contrast agents, according to Kavaliauskiene. Usually they have low signal intensity on T1-weighted images (optimizing the contrast between the enhancing bowel wall and hypointense lumen) and high signal intensity on T2-weighted images. Mannitol with tap water is often used as a biphasic agent. Intravenous contrast agents (gadolinium 0.1 ml/kg) are recommended for the assessment of inflammation of the small bowel and can be helpful for diagnosing other small bowel diseases as well.
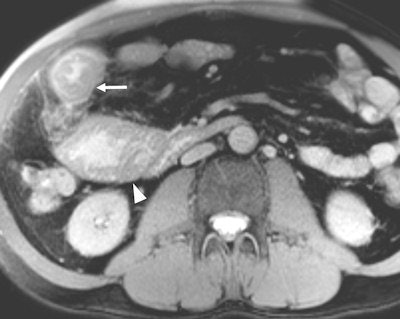 A 56-year-old patient with Crohn's disease presented with a worsening clinical condition spanning three months. Active Crohn's disease was suspected clinically. MR enterography axial fat-saturated true-FISP image demonstrates circumferential irregular small bowel wall thickening -- tumor with adjacent fat infiltration (white arrow) and prestenotic bowel dilatation (arrowhead). MRI findings demonstrated a small bowel primary tumor as a cause of the symptoms; histopathology revealed adenocarcinoma. There was no evidence of active Crohn's disease.
A 56-year-old patient with Crohn's disease presented with a worsening clinical condition spanning three months. Active Crohn's disease was suspected clinically. MR enterography axial fat-saturated true-FISP image demonstrates circumferential irregular small bowel wall thickening -- tumor with adjacent fat infiltration (white arrow) and prestenotic bowel dilatation (arrowhead). MRI findings demonstrated a small bowel primary tumor as a cause of the symptoms; histopathology revealed adenocarcinoma. There was no evidence of active Crohn's disease.Peritonitis, or serositis, of small bowel loops may occur in common diseases causing acute abdominal pain (e.g. appendicitis), in postsurgical patients and in rarer diseases such as familial Mediterranean fever, Kavaliauskiene wrote. This is a hereditary autosomal recessive disease with the highest prevalence in Turkey and lower prevalence in Israel, Armenia, and other Middle East countries. The fever is also found in Greece, North Africa, Italy, Germany, France, the U.S., and Japan. The prevalence of the gene associated with familial Mediterranean fever mutation in different ethnographic groups predisposes such distribution. Distribution is related to world migration as most ancient mutations appeared in the Middle East -- in the former area of Mesopotamia -- and are thought to be spread all over the world.
The authors acknowledged the support of the European School of Radiology (ESOR) and the European Society of Gastrointestinal and Abdominal Radiology (ESGAR) in this research. When writing the manuscript, Kavaliauskiene was ESOR/ESGAR fellow at the Academic Medical Center, University of Amsterdam.