Most radiologists have heard of Moore’s Law. It was named after Gordon Moore, co-founder of Intel. In 1965, he observed that the number of components on a microchip had been doubling every year. He also predicted that this would continue for at least ten years. In 1975, he revised this to every two years. Rather oddly, this has been uncannily accurate for the intervening 50 years.
A close colleague observed that radiologists are affected by a type of Moore’s Law. The amount of scans a radiologist is expected to shift per day is increasing year on year. Not doubling every two years but expectations are steadily growing. Today’s radiologist is expected to shift work at an eye-watering rate. Our forebears would weep at the modern pressure of expectations.
 Dr. Paul McCoubrie.
Dr. Paul McCoubrie.
When I was in short medical trousers, I grew up surrounded by mighty plain film gods. They would sit at the banks of lightboxes, their hands in constant motion as the films went up and down in a fluid motion, merely skimming over the brightly illuminated surfaces, staying still for a few split seconds as the report was barked onto tape.
And they did this alarming juggling act for hour after hour, day after day, demolishing huge piles of film packets. Some of my radiological heroes would report a staggering 30,000 to 40,000 radiographs a year. I still don’t know how they did it. Well, apart from an impeccable work ethic and having done it so often, they were operating on basal ganglia most of the time. The neocortex rarely had to engage. They truly were on autopilot.
Then CT and MR went mainstream. But they were thankfully slow. Does anyone remember scanners that took a minute per single slice? 20s rotation, 40s reconstruction. To cover a CT and MR "list" was a luxury; it was to escape the murderous fluoroscopy rooms, intravenous urography (IVU) lists, and indeterminable piles of plain films.
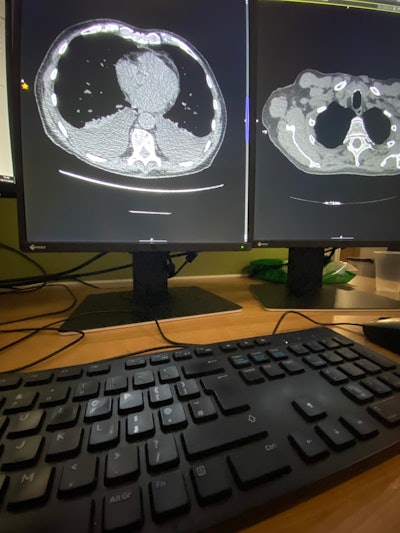 What most radiologists see: all day, every day. Image courtesy of Dr. Paul McCoubrie.
What most radiologists see: all day, every day. Image courtesy of Dr. Paul McCoubrie.
Then the scanners got fast. The scanners could reconstruct images faster than we could report them. Scanners operated early morning, late evening, and at the weekends. More scanners were installed but few radiologists were employed. Slowly but surely scanning capacity was divorced from reporting capacity. I remember the crossing of this particular radiological Rubicon about 15 years ago here in the U.K.
So what happened? Well, radiologists had to up their game. They had to report faster and work longer hours. But that only butters so many parsnips -- particularly in the U.K. National Health Service (NHS), where radiologists are salaried and have decent employment rights, so their monopsony employer could only thrash them lightly. Those who are paid by the scan were not spared the managerial birch twigs.
So radiologists started dropping duties. So as to report more CT and MRI, radiologists stopped doing hands-on ultrasound and fluoroscopy. Some even [startled gasp] gave up reporting plain radiographs. Many diagnostic radiologists became pure CT and MRI specialists.
Radiologists also stopped doing paperwork. They stopped vetting and protocolling scans. They stopped checking their reports. This was all delegated. They were pure lean, mean CT reporting machines.
But the pressure kept building, and the number of CT and MRI scans grew by 20% annually in my hospital. Radiologists then started a new tactic: hiding. The only way they could appease the gods of cross-sectional imaging was to avoid contact with other humans. By locking doors, retreating to hard-to-find PACS stations, giving up clinical meetings, and not answering phones or emails, radiologists found they could get more cross-sectional done. Working from home ticked all these boxes. Radiologists got called antisocial, rude, and grumpy, but they could cope with that so long as the CTs and MRIs got read.
And yet the workload expectation grew. The next tactic that radiologists used to cope with their burgeoning workload was ergonomics. It is true that productivity can be improved by improving the environment in which a radiologist works. The advent of sit-stand desks, mandatory air conditioning, 4-point adjustable chairs, and voice-recognition software that actually worked all made a small improvement to productivity.
But expectations have grown. A good day five to 10 years ago was reporting 40 cross-sectional imaging studies. You’d be happy with that, walk out with a spring in your step, a solid day’s work behind you. Now that would be an average day. It is not unusual to hear of radiologists expected to report 70+ scans a day. This entails a 10- to 12-hour day, five days a week.
When you sit back and look at what has happened to radiology over the last twenty years, how much it has changed and it’s all about servicing the massive burden of CT and MRI reporting. Some of this is, of course, good. We understand so much more about the human body, disease, and how to detect it accurately via cross-sectional means.
But we’ve ripped the heart of what it means to be a radiologist. Gone are the polymaths, the generalists who can turn their hand to anything. Gone is any semblance of control over our workflow. Gone is the popular and approachable radiologist that clinicians would seek to discuss cases.
And it’s caused an epidemic of burnout. Barreling through CT and MRI scans like a video game, barely looking at the images purely to get on to the next case, isn’t why we became doctors. It’s almost entirely devoid of meaning and singularly lacking in fulfillment. No wonder radiologists are browned off.
The worst thing about it? We’ve been played. It happened right in front of us, on our watch. We’ve been taken for suckers. And it is going to be mighty hard to stop or even reverse the radiological Moore’s Law of reporting. Or as I shall name it, Kelly’s Rule of Radiology Reporting, after my friend Barry Kelly who got me onto this topic.
But stop this we must. It is unsustainable. It is unsafe for our patients. It is absolutely ripping the heart out of our beautiful specialty. Quite how we do so is another question.
Dr. Paul McCoubrie is a consultant radiologist at Southmead Hospital in Bristol, U.K. Competing interests: None declared.
His new book -- More Rules of Radiology -- is available via its publisher Springer and also local bookstores ( ISBN-13 978-3031640933).
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.




















