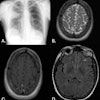
A detailed new whole-body MRI study has revealed that patients who are hospitalized for COVID are three times more likely to have some abnormalities in multiple organs, particularly the lungs, brain, and kidneys. Researchers think there is a link with the severity of the illness.
The study, published on 22 September in Lancet Respiratory Medicine, looked at 259 patients across 13 U.K. sites who were discharged from hospital with polymerase chain reaction (PCR)-confirmed or clinically diagnosed COVID-19 between 1 March 2020 and 1 November 2021. The mean age was 57 years, and 158 (61%) were male and 101 (39%) were female.
Five months after the patients were discharged, MRI scans of their major organs showed some significant differences when compared with 52 non-COVID-19 controls from the community (mean age, 49; 30 [58%] male and 22 [42%] female).
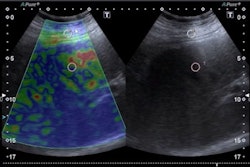
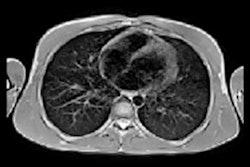
The biggest impact was seen on the lungs, where the scans were 14 times more likely to show abnormalities. MRI scans were also three times more likely to show some abnormalities in the brain -- and twice as likely in the kidneys -- among people who had had severe COVID. There was no significant difference in the health of the heart or liver.
"The patient's age, how severely ill they were with COVID, as well as if they had other illnesses at the same time, were all significant factors in whether or not we found damage to these important organs in the body," Dr. Betty Raman, associate professor of cardiovascular medicine from the Oxford Centre for Clinical Magnetic Resonance and a lead investigator for the study, told BBC News.
The presence of lung MRI abnormalities was associated with a twofold higher risk of chest tightness, and multiorgan MRI abnormalities were associated with severe and very severe persistent physical and mental health impairment after hospitalization, the researchers noted.
They found that some symptoms matched up with signs of organ damage revealed by the MRI scans -- for example, a tight chest and cough with abnormalities in the lungs. However, not all of the symptoms experienced by those living with long COVID could be directly linked to what was seen on the scans.
A summary of the key clinical characteristics of patients that were associated with single-organ injury, including follow-up clinical measures. ACR = albumin to creatinine ratio. BNP = B-type natriuretic peptide. CRP = C-reactive protein. eGFR = estimated glomerular filtration rate. EQ-5D-5L = EuroQol 5-level. FVC = forced vital capacity. KCO = carbon monoxide transfer coefficient. LFT = liver function test. OR = odds ratio. PHQ-9 = Patient Health Questionnaire-9. TLCO = transfer factor of the lung for carbon monoxide. * = Associations present after excluding patients with corresponding organ comorbidities. † = Association only present after excluding patients with corresponding organ comorbidities.
Raman said it also seems that abnormalities in more than one organ were more common among people who had been admitted to hospital and were still reporting physical and mental health problems after they had recovered from the initial infection.
"What we are seeing is that people with multiorgan pathology on MRI -- that is, they had more than two organs affected -- were four times more likely to report severe and very severe mental and physical impairment," she told BBC News.
The findings are part of a bigger study looking at the long-term effects of COVID on those who were hospitalized, known as the Post-hospitalisation COVID-19 study (PHOSP-COVID). The results highlight the need for longer-term multidisciplinary follow-up services focused on pulmonary and extrapulmonary health (kidneys, brain, and mental health), particularly for those hospitalized for COVID, according to Raman.
"It is abundantly clear now that it (COVID) is not simply a respiratory virus," Dr. Margaret O'Hara, a founding trustee of Long Covid Support, said to Sky News. "It is causing long-term harm to the health of individuals throughout the population, including the huge numbers of people who were not hospitalized in the acute phase of infection."
You can read the full Lancet Respiratory Medicine article by clicking here.