More than half of children affected by stroke receive a delayed diagnosis -- typically between 12 and 24 hours after it occurred -- and 10% of them get no diagnosis at all, according to a leading Spanish expert.
 Dr. Yolanda Ruiz Martín. Courtesy of SERAM.
Dr. Yolanda Ruiz Martín. Courtesy of SERAM.The false belief that strokes do not affect children and the low availability of MRI are two of the contributing factors, said Dr. Yolanda Ruiz Martín, a pediatric radiologist at the Hospital General Universitario Gregorio Marañón in Madrid, at the Spanish Society of Medical Radiology (SERAM) annual congress, which drew to a close on 26 May.
She pointed out that there is "a real lack of knowledge" of pediatric stroke and that "we must increase the suspicion index of stroke among parents and doctors" in order to avoid late diagnosis. She believes that the implementation of clinical guidelines, protocols, and stroke codes will help to raise awareness.
Ruiz Martín explained that there is a delay in the inclusion of children in the "Stroke Code" due to a lower incidence compared with adults and due to the lack of prospective randomized trials. Her hospital is one of three (together with the 12 de Octubre and La Paz hospitals) that the Community of Madrid designated as reference sites in pediatric "Ictus Code" in 2019. Since then, 35 children with suspected stroke have been treated at the Gregorio Marañón University General Hospital.
Lifelong neurological sequelae
Ruiz Martín said there is a belief that pediatric stroke has a good prognosis due to neuronal elasticity, but she clarifies that this is not true. "10% of children die, 20% will have recurrences, and 75% will have lifelong neurological sequelae," she noted. "We are talking about children with a whole life ahead of them, living with a disability that bears a high social and economic cost."
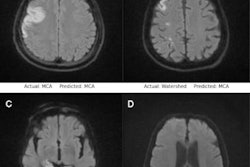
MRI is the imaging test that most reliably determines a pediatric stroke, and it must be available 24/7 at the reference centers, she continued. Only in exceptional circumstances, such as MRI being unavailable due to breakdown or for patients who cannot undergo MRI, should CT with angio CT be performed.
Ruiz Martín noted that 73% of acute neurological deficits in adults will be infarcts, and that in most cases the clinical manifestations together with CT or angio CT images are sufficient to diagnose and treat stroke. However, in children, only 7% of these deficits are going to be strokes, with the remaining possibly being migraines and a very diverse range of different diseases, she added. Stroke may also present with headaches and alterations in consciousness.
All this results in a fairly high percentage of children having stroke simulators that CT is not able to differentiate; normal CT is not sensitive to early ischemia in children and often gives us a false sense of reassurance, which contributes to a substantial delay in the diagnosis of infarction, she said.
Risk factors and treatments
For the pediatric radiologist, almost as urgent as diagnosing the infarction is establishing its etiopathogenesis, since the treatment will be very different in each case. In this respect, Ruiz Martín assured the virtual SERAM delegates that MRI is also the radiological test that is going to be most helpful.
The risk factors in children are numerous and different from those in adults, and the cause will more often be multifactorial and almost always the responsible etiological factor will be found, she said.
The Childhood AIS Standardized Classification and Diagnostic Evaluation (CASCADE) criteria was established in 2012 to standardize the classification and diagnosis of pediatric arterial ischemic infarction.
These are four types of arteriopathies -- the most frequent among all the risk factors, especially with regard to a previously healthy child, according to Ruiz Martín. They are associated with upper airway infections and colds in previous days, increasing the risk of infarction by up to 6.3 times. One subtype is postchickenpox arteriopathy, which can occur if the child has had chickenpox in the 12 months prior to the infarction. It should also be taken into account that 30%-50% of arterial dissections can be caused by minor trauma, she said.
Another common arteriopathy is calciform cell anemia, which entails a risk of infarction similar to that of adults and requires a very early diagnosis before an urgent exchange transfusion to the child can be performed.
Other risk factors can be cardioembolism, which usually occurs if the child has congenital or acquired heart disease or has undergone cardiac surgery or intervention. Finally, there are cases of undetermined as well as multifactorial etiology. The latter may occur in children with hematological, genetic, or metabolic diseases, she concluded.
Editor's note: This article is based on an article in Spanish posted on 26 May by SERAM. Translation by Jana Santiburcio of the European Board of Radiology.