Abnormal previous imaging in cases of unexplained and unintentional weight loss may be useful to fast-track patients for CT scans, but questions remain unanswered and further work must be done in this area, according to Scottish researchers.
"Unexplained and unintentional weight loss can be a worrying sign of malignancy for which CT is increasingly being used to investigate. However, it is a frequent symptom, especially in the elderly, which may be idiopathic, due to benign disease, or linked to social causes," explained Dr. Eilidh Bell and colleagues from Aberdeen Royal Infirmary and Forth Valley Royal Hospital in Larbert.
In addition, blind CT imaging is not without drawbacks, including potentially unnecessary radiation exposure, high cost, and incidental findings, they added in an e-poster presentation at the 2018 Annual Scientific Meeting of the U.K. Royal College of Radiologists (RCR) in Liverpool, U.K.
The authors hypothesized that diagnostic and malignancy rate would be low in patients with normal previous imaging, primarily chest x-ray and abdominal ultrasound, which could be used to avoid unnecessary CT scans. Their main aim was to investigate the association between previous imaging results and diagnostic and malignancy rates, and also they wanted to investigate the association between previous imaging results and mortality, plus the association between symptoms and diagnostic yield.
The team conducted a retrospective study of CT scans done at Forth Valley Royal Hospital during 2013. A total of 557 CTs were performed for unexplained and unintentional weight loss, which they defined as weight loss without features suggestive of a specific diagnosis.
They categorized patients based on the results of previous chest x-ray and abdominal ultrasound exams carried out in the three months prior to the CT scan. CT examinations were deemed "positive" if they found or directly lead to investigations that discovered a cause of unexplained weight loss. The data included demographics, previous imaging, and request information, which were collected using electronic records. Additional symptoms were collected from CT request information.
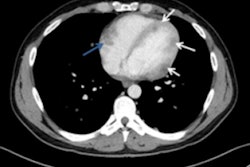
 Frequencies of malignancies found in unexplained and unintentional weight loss.
Frequencies of malignancies found in unexplained and unintentional weight loss.Patients with abnormal previous imaging had higher diagnostic (p < 0.05), malignancy (p < 0.05), and mortality (p < 0.05) rates than those with normal or no previous imaging. No difference was found in diagnostic, malignancy, or mortality rates between patients with normal imaging and those with no previous imaging. The presence of or number of symptoms other than weight loss did not affect diagnostic (p < 0.05) or malignancy rates (p < 0.05).
Overall, the authors noted a considerable malignancy rate, even in those with normal (9.2%) or no previous imaging (5.9%).
"Abnormal previous imaging is significant, however, normal chest x-ray and/or abdominal ultrasound or lack of additional symptoms prior to CT examination is not reassuring in unexplained and unintentional weight loss," they wrote.
Bell is also a keen advocate of using handover sheets to provide valuable information about patients, ensuring continuity of care. When no guidance is given on the contents of these sheets, they often contain inaccurate, out-of-date information, she wrote in a 2017 poster in BMJ Leader. Frustrated by the squandering of a potentially useful tool, she attempted to create an organized handover sheet by participating in a quality improvement project and developing a template inserted into the sheet that provided essential information in a more structured format.
"The main issue is maintaining an accurate handover during receiving weeks. To improve this, an interruption-free period for one staff member each evening during this week is being trialed," Bell stated. "I hope to inspire junior healthcare professionals to effect change. The best ideas can come from a fresh pair of eyes. Improving healthcare doesn't have to mean enormous plans; a simple idea can lead to positive results in patient care."
Second study on weight loss
Weight loss was by far the most common presenting symptom in another study presented at the RCR congress in Liverpool, in which researchers from St. Helens and Knowsley Teaching Hospitals National Health Service (NHS) Trust investigated the use of CT in the chest, abdomen, and pelvis in patients with nonspecific symptoms suspicious for malignancy of undefined origin.
"In our hospital, a suspected malignancy of undefined origin pathway has been piloted in conjunction with the local primary care and oncology team whereby all patients with suspected malignancy of undefined origin undergo minimum baseline tests, including blood tests, urinalysis, and chest x-ray before having CT if no obvious primary cancer site is identified," explained authors Drs. C. Kan and J. Wide.
They sought to determine the detection rate of malignancy identified using CT in patients with nonspecific symptoms by assessing all 134 scans CT scans of the chest, abdomen, and pelvis performed between October 2016 and September 2017 at a large district general hospital. The exclusion criteria were scans performed for other reasons, patients with abnormal preliminary imaging, raised tumor markers, abnormal clinical examination findings, and known/previous malignancy.
Kan and Wide reviewed all included scan reports and images. Indicated presenting symptoms, preliminary blood test abnormalities, social history, and family history were identified from the clinical details provided in the scan request.
All patients were general practitioner referrals, and the mean age was 69 (range, 41 to 92), and 77 were female. A total of 109 (81.3%) scans were normal, while 25 (18.7%) were abnormal. Among the abnormal scans, six (4.5%) showed definite malignancy, while 19 (14.5%) had equivocal findings. The indeterminate scans were followed-up six to 12 months later via electronic medical records, which showed no additional definite malignancies.

The proportion of malignancy ultimately diagnosed was 4.5%. The most common presenting symptoms were weight loss, fatigue, abdominal pain/tenderness, and poor appetite. Other common indications include anemia, raised inflammatory markers, and a history of smoking.
"The detection rate of malignancy using CT in patients with nonspecific symptoms suspicious for malignancy of undefined origin in the study is low," noted the authors, adding it is uncertain what is considered an acceptable rate for a screening study. "The incidence of malignancy rises with age significantly in later life and it is unclear what would be the incidence in a similar control population."
There is poor correlation between presenting symptoms alone and the presence of malignancy, they continued. There is certainly an overlap with nonmalignant conditions such as connective tissue diseases, and patients may be referred between special multidisciplinary and rheumatology teams. Also, the study identified three lung cancers and one abnormal thymic tissue, suggesting that chest inclusion is appropriate.
Although the incidence of malignancy is low, CT of the chest, abdomen, and pelvis is probably acceptable for patients with nonspecific symptoms after baseline tests, but not as a first-line investigation, Kan and Wide concluded.