The use of a streamlined MRI protocol could help reduce unnecessary biopsies by as much as 30% in men suspected of having prostate cancer, according to a study published online on June 8 in JAMA Network Open.
The approach, called biparametric MRI (bpMRI), uses fewer MRI sequences -- potentially decreasing image acquisition time to approximately 15 minutes -- and achieves diagnostic accuracy without the need for intravenous contrast, wrote a group led by Dr. Lars Boesen, PhD, from Herlev and Gentofte University Hospital in Herlev, Denmark.
Typically, men with elevated prostate-specific antigen (PSA) levels are sent on for biopsy, but PSA screening is controversial and has a high false-positive rate. Imaging tools such as multiparametric MRI (mpMRI) are used to identify which candidates might have prostate cancer and are suitable for targeted biopsy, but mpMRI can be time-consuming, it uses contrast, and it can be difficult to implement, the researchers wrote.
Biparametric MRI offers the possibility of a simpler, faster protocol with no contrast and the same accuracy as mpMRI in terms of determining who should be sent on for targeted biopsy, according to the group. To test the protocol, the researchers evaluated 1,020 men suspected of having prostate cancer. The subjects had a median age of 67 years (range: 61-71 years) and a median PSA level of 8 ng/mL (range: 5.7-13 ng/mL).
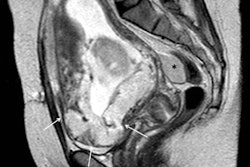
The subjects were first scanned on a 3-tesla MRI system (Philips Healthcare) with a phased-array coil positioned over the pelvis. The bpMRI protocol included T2-weighted and diffusion-weighted imaging.
All men then received standard transrectal ultrasound-guided (TRUS) biopsies, and the bpMRI results were consulted to see which men should receive additional targeted biopsy.
Boesen and colleagues compared the use of standard biopsy in all subjects with standard plus targeted (combined) biopsy only in those with suspicious findings on bpMRI. By restricting combined biopsy to men with suspicious bpMRI results, 305 (30%) men with a low suspicion of prostate cancer could avoid prostate biopsy (p < 0.001), the group found.
The number of significant prostate cancer diagnoses increased by 11% (p < 0.001), while the number of insignificant prostate cancer diagnoses decreased by 40% (p < 0.001), they wrote. The negative predictive value (NPV) of bpMRI for ruling out significant cancer was 97%.
"This study showed that a low-suspicion bpMRI had a high NPV in ruling out significant prostate cancer in confirmatory biopsies," the authors concluded. "The results suggest that bpMRI may be used as a triage test to exclude the presence of aggressive disease and avoid unnecessary biopsies with its inherent complications."