
Stress echocardiography is as effective and cheaper than direct referral to invasive coronary angiography in chest pain patients with a high pretest probability of coronary artery disease -- and appears competitive with rival coronary CT angiography (CCTA) as an initial exam, according to a new study in the BMJ's Open Heart.
In their study, Dr. Alexandros Papachristidis and colleagues from King's College in London performed stress echocardiography in chest pain patients with a high pretest probability (greater than 61%) of coronary disease, referring them for invasive coronary angiography (ICA) when appropriate. Comparing cost-effectiveness between initial stress echo and direct referral to the cath lab, they found initial stress echo to be cheaper overall by about 745 pounds (853 euros), with a very low rate of adverse events over 12 months (Open Heart, 15 June 2017).
"Our study demonstrates that an imaging-first strategy, i.e., stress echo, in patients with high pretest probability of coronary artery disease, is cost-effective and appears safe," Papachristidis, who is an echocardiography fellow, wrote in an email to AuntMinnieEurope.com.
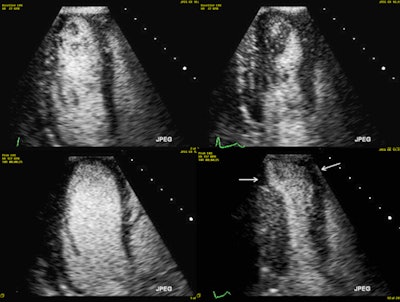 Exercise stress echocardiography with ultrasound contrast agent. Top row: Rest images in diastole (left) and systole (right; there is some contrast swirling due to lower cardiac output at rest). Bottom row: Peak stress images in diastole (left; note the dilatation of the left ventricle) and systole (right; note that the apical segments become severely hypokinetic -- white arrows). All images courtesy of Dr. Alexandros Papachristidis.
Exercise stress echocardiography with ultrasound contrast agent. Top row: Rest images in diastole (left) and systole (right; there is some contrast swirling due to lower cardiac output at rest). Bottom row: Peak stress images in diastole (left; note the dilatation of the left ventricle) and systole (right; note that the apical segments become severely hypokinetic -- white arrows). All images courtesy of Dr. Alexandros Papachristidis.Conflicting advice
Updated guidelines recommend the use of a functional test before invasive angiography in these patients, but CCTA has been the preferred test of late, with stress echo relegated to the sidelines.
The U.K. National Institute for Health and Care Excellence (NICE) published guidelines on stable chest pain in 2010, recommending invasive angiography in patients with high pretest probability of coronary disease.
The European Society of Cardiology (ESC), on the other hand, recommended an initial functional imaging test, such as stress echocardiography, for patients with pretest probability of 15% to 85%, or greater than 85% under certain circumstances. And the newest NICE update recommends skipping the probability score in favor of initial CCTA for everyone, the group noted.
In 2016, the Clinical Evaluation of Magnetic Resonance Imaging in Coronary Heart Disease 2 (CE-MARC 2) trial showed that stress cardiac MR and nuclear stress used in these patients reduced the need for coronary angiography without increasing adverse events.
In their study, the researchers assessed the clinical and cost-effectiveness of stress echo in patients with new-onset chest pain and high pretest probability of coronary artery disease, the group wrote.
The study began with 594 consecutive patients with new-onset chest pain who underwent stress echo over a year. Calculating pretest probability based on U.K. NICE guidelines, 257 patients had a score of 61% or greater, suggesting a high pretest probability of coronary disease, and for whom the U.K. NICE guidelines recommends direct referral to coronary angiography. The researchers analyzed the results from this group for their study.
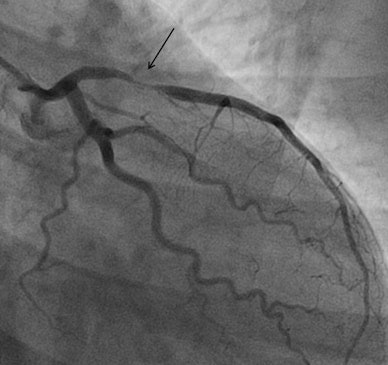 Invasive coronary angiography of the same patient. The black arrow shows a very tight narrowing in the proximal left anterior descending artery.
Invasive coronary angiography of the same patient. The black arrow shows a very tight narrowing in the proximal left anterior descending artery.They used the Bruce treadmill exercise protocol for the exercise stress echo, aiming to reach the maximum predicted heart rate. Standard images were acquired at rest and immediately after peak exercise. For the dobutamine stress echo, they used the standard 3 min stages protocol with incremental dobutamine doses of 5, 10, 20, 30 and 40 µg/kg/min. Ultrasound contrast was administered if at least two myocardial segments weren't seen on baseline echo images.
The researchers recorded follow-up data for 12 months with regard to major adverse cardiac and cerebrovascular events, documenting any late revascularization for acute coronary syndrome/unstable angina, myocardial infarction, cardiovascular death, and stroke.
Cheaper with pretest?
To calculate costs, the group added the costs of stress echo (300 pounds, 340 euros) plus invasive angiography when performed (1,400 pounds, 1,602 euros) for all patients, dividing the total cost by the number of patients to arrive at average costs. The costs of their strategy was compared with the hypothetical cost of direct referral to angiography.
In all, 210 of 257 (81.7%) of the high-pretest probability patients had dobutamine stress echo, while 18.3% had an exercise stress echo. All tests reached high heart rates, and the researchers found no adverse events, though two patients had hypotension at the peak of dobutamine stress, and one developed atrial fibrillation.
A total of 106 patients (41.2%) had a positive stress echo, and 61 underwent invasive angiography, in which 15 (24.6%) were revascularized. The average cost per patient for all studies was 654 pounds (748 euros). If NICE guidance had been followed, the costs would have been significantly higher at 1,400 pounds (1,602 euros), a difference of 746 pounds (853 euros).
"Our registry of 257 patients demonstrates that stress echo is clinically effective, reduces the cost of investigations by reducing the need for invasive coronary angiography, and appears to be safe with only two myocardial infarctions recorded in a 12-month period, both in patients with a positive stress echocardiogram," Papachristidis told AuntMinnieEurope.com.
The follow-up period of the current study was relatively short, identical to the CE-MARC 2 trial, but there were very few events recorded to draw certain conclusions, he added. Interestingly, in the coronary angiography arm of the CE-MARC 2 trial of 240 patients, there were two myocardial infarctions as well.
Evolving recommendations
NICE has changed its guidelines on stable chest pain dramatically since publication six years ago, and in doing so departed dramatically from the previous standard of care, the exercise ECG, they wrote. NICE seeks the most cost-effective strategy to evaluate patients with chest pain, and it could have a big impact in clinical practice because the U.K. has 49 centers that perform CCTA, whereas 120 of 198 echocardiography departments in the U.K. perform stress echo.
"The question for cardiology departments with established or recently expanded functional imaging services is whether to downsize these departments and expand cardiac CT instead," the authors wrote.
There will certainly be false-negative tests with initial noninvasive tests, and CCTA does a good job as well -- with an initial sensitivity of 81% and a negative predictive value of almost 97%, they noted. But the CCTA-first strategy has been criticized. Moreover, for patients with high pretest probabilities, a negative noninvasive test may not be able to conclusively rule out coronary disease. Yet, noninvasive tests are attractive because they can reduce complications, are widely available, and can reduce the time to diagnosis, the study team noted.
Stress echo remains a low-cost and readily available modality to investigate patients with new onset chest pain and high pretest probability of coronary artery disease, the authors concluded. It can reduce the cost of workup substantially in these high-risk patients. However, this study lacks the statistical power to make conclusions about its efficacy and safety. The data do not show a clear signal of harm, but the possibility cannot be ruled out, Papachristidis and colleagues wrote.
"In fact, either CCTA or stress echo/functional imaging tests are clinically a better way than going straight to invasive angiography, and the question is which will be the lower cost and also safer option," they stated. "CCTA has a high negative predictive value but involves radiation, which needs to be taken into account especially in young age populations."
Moreover, a large recent CCTA-first trial, the Prospective Multicenter Imaging Study for Evaluation of Chest Pain (PROMISE), showed a higher rate of invasive angiography (13.3% versus 5.1%) with CCTA without improving clinical outcomes, Papachristidis noted. On the other hand, stress echo can provide a lot of prognostic information especially when combined with treadmill exercise, he wrote.
The researchers are currently investigating the cost-effectiveness of the two tests. In one institution, the 2016 updated NICE guidance is followed and in another institution they are investigating high pretest probability patients with stress echo initially.
"This is not a randomized trial but will shed more light to the question" of CCTA or stress echo on a real-life basis, he concluded.



















