
Prompt diagnosis of pseudoaneurysms is essential because the unpredictable associated complications carry high morbidity and mortality rates, and a proper knowledge of embolization materials and percutaneous techniques is vital for the management of pseudoaneurysms and to choose the appropriate treatment, an award-winning research team from Spain has found.
Pseudoaneurysms are common vascular abnormalities that represent a disruption in arterial wall continuity resulting from inflammation, trauma, or iatrogenic causes. In the last few years, their frequency has increased due to the growth of endovascular procedures and the advent of new noninvasive imaging techniques with high sensitivity for their detection, noted Dr. Virgilio Benito Santamaria and colleagues from the department of radiology at Hospital de la Santa Creu i Sant Pau in Barcelona.
"It is generally agreed that symptomatic pseudoaneurysms should be treated," they wrote in an education exhibit that won a Magna Cum Laude at last month's RSNA meeting in Chicago. "The decision to treat asymptomatic pseudoaneurysms is controversial since spontaneous thrombosis of the pseudoaneurysm is known to occur; we cannot predict which pseudoaneurysm will undergo spontaneous thrombosis."
The location of the pseudoaneurysm may affect its outcome. Some experts recommend observing small asymptomatic pseudoaneurysms and treating them only if they enlarge, do not resolve, or become symptomatic, but the risk of spontaneous rupture of extraorganic visceral pseudoaneurysm is very high, regardless of their size, and it is correlated with a high mortality rate that may approach 100%, they explained. Therefore, some authors believe that definitive treatment should be performed in all such cases.
A full clinical evaluation of the patient is essential, and information about the etiology of the pseudoaneurysm, hemodynamic stability, and anticoagulation therapy is important. Studying the characteristics of the pseudoaneurysm is important, including anatomical localization, the size of the pseudoaneurysm sac, size of surrounding hematoma, diameter of pseudoaneurysm neck, vascular territory (superficial or deep/visceral) that the pseudoaneurysm arises from, and the type of end artery (expendable or inexpendable) in which the pseudoaneurysm is located. Ultrasound and CT angiography can determine all these features, although conventional angiography is used most of the time as a prelude to endoluminal treatment of the pseudoaneurysm, they stated.
"In brief, a complete work-up to determine the cause and location of the pseudoaneurysm and to evaluate surrounding structures and relevant vascular anatomy is essential in the selection of the treatment technique," continued Santamaria and colleagues. "Treatment options should be tailored to the location, morphological features, rupture risk, and clinical setting of the pseudoaneurysm and to any patient comorbidities.
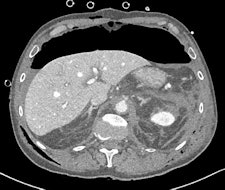
 Gastroduodenal artery pseudoaneurysm in a 45-year-old man with pancreatitis and upper gastrointestinal bleed. Image courtesy of Dr. Paresh K. Desai and radiopaedia.org.
Gastroduodenal artery pseudoaneurysm in a 45-year-old man with pancreatitis and upper gastrointestinal bleed. Image courtesy of Dr. Paresh K. Desai and radiopaedia.org. radiopaedia.org/cases/gastroduodenal-artery-pseudoaneurysm.
A false aneurysm -- another term for a pseudoaneurysm -- is when there is a breach in the vessel wall such that blood leaks through the wall but is contained by the adventitia or surrounding perivascular soft tissue, according to Dr. Yuranga Weerakkody and Dr. Donna D'Souza et al, writing on radiopaedia.org. A direct communication of blood flow exists between the vessel lumen and the aneurysm lumen through the hole in the vessel wall. The risk of rupture is higher than that of a true aneurysm of comparable size due to poor support of the aneurysm wall, and thus false aneurysms generally require treatment.
They note the causes include trauma (dissection or laceration); iatrogenic (dissection, laceration, or puncture), e.g., arterial catheterization (accounts for most cases in this category), biopsy, surgery; spontaneous dissection; fibromuscular dysplasia (dissection); mycotic aneurysm (inflammatory digestion of the vessel wall); myocardial infarction (left ventricular false aneurysm); regional inflammatory process (acute and chronic pancreatitis); vessel injury/erosion due to a tumor (relatively uncommon); vasculitides (Behcet syndrome, giant cell arteritis, Takayasu arteritis, systemic lupus erythematosus, polyarteritis nodosa); and penetrating atherosclerotic ulcer.

 Left: CT performed after laparotomy. Retroperitoneal hematoma in the upper abdomen surrounds the abdominal aorta also involves left perirenal space with thickening of pararenal fascia. A 3.5 mm outpouching from the left lateral wall of the upper abdominal aorta just inferior to the level of the coeliac axis (L1 level) is located short distance anterior to a tiny arterial branch. This is the epicenter of the upper abdominal hematoma and may represent small false aneurysm either from traumatic transection or at the site of avulsion of a small aortic branch. No intimal dissection flap is identified. A large volume pneumoperitoneum is also present. Right image: Repeat CT angiography a week later demonstrated spontaneous thrombosis of the tiny false aneurysm. Image courtesy of Dr. Andrew Lawson and radiopaedia.org. radiopaedia.org/cases/traumatic-abdominal-aortic-false-aneurysm.
Left: CT performed after laparotomy. Retroperitoneal hematoma in the upper abdomen surrounds the abdominal aorta also involves left perirenal space with thickening of pararenal fascia. A 3.5 mm outpouching from the left lateral wall of the upper abdominal aorta just inferior to the level of the coeliac axis (L1 level) is located short distance anterior to a tiny arterial branch. This is the epicenter of the upper abdominal hematoma and may represent small false aneurysm either from traumatic transection or at the site of avulsion of a small aortic branch. No intimal dissection flap is identified. A large volume pneumoperitoneum is also present. Right image: Repeat CT angiography a week later demonstrated spontaneous thrombosis of the tiny false aneurysm. Image courtesy of Dr. Andrew Lawson and radiopaedia.org. radiopaedia.org/cases/traumatic-abdominal-aortic-false-aneurysm."They can involve any arterial segment or even a cardiac chamber. Examples include femoral artery pseudoaneurysm (relatively common site due to femoral punctures), carotid artery pseudoaneurysm, visceral arterial pseudoaneurysm, peripheral arterial (limb) pseudoaneurysm, left ventricular pseudoaneurysm, and brachiocephalic artery pseudoaneurysm," wrote Weerakkody and D'Souza. "Some of the imaging features may be dependent on location. Due to the turbulent forward and backward flow, a characteristic yin-yang sign may be seen on color flow, while a 'to and fro' pattern may be seen with pulsed Doppler."



















