
Researchers from Rome have collected a top award for their e-poster about CT of peritoneal carcinomatosis. Judges at this month's European Congress of Radiology (ECR) commended them for revealing the spectrum of diagnostic patterns and the sites involved in this condition, and for proposing a new reporting scheme for dealing with future cases.
Knowledge of patterns of peritoneal carcinomatosis and sites most frequently involved is crucial for radiologists, and a workable reporting scheme is necessary to direct a report and provide a description of the disease, according to lead author Dr. Maria Ciolina, from the department of radiological sciences, Sapienza University of Rome, Italy. Also, an effective pretreatment approach to peritoneal carcinomatosis requires an accurate staging with detailed information about the number of implants and sites involved.
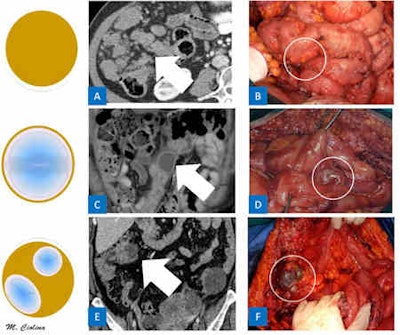 Different aspects of peritoneal implants. A: Axial contrast-enhanced CT scan shows solid implants (arrow) presenting as several homogenous soft-tissue nodules. B: Intraoperative image of solid implants (circle). C: Coronal contrast-enhanced CT image shows cystic implant (arrow) over small bowel loops appearing hypodense due to the internal fluid component. D: Intraoperative image of cystic implants (circle). E: Axial contrast-enhanced CT image shows 4-cm implant of peritoneal carcinomatosis (arrow) presenting as an ovular shape and a mixed structure consisting of a mucinous cystic component and a solid irregular rounded wall showing contrast enhancement. F: Intraoperative image of mixed implants (circle). All images courtesy of Dr. Maria Ciolina and Dr. Andrea Laghi.
Different aspects of peritoneal implants. A: Axial contrast-enhanced CT scan shows solid implants (arrow) presenting as several homogenous soft-tissue nodules. B: Intraoperative image of solid implants (circle). C: Coronal contrast-enhanced CT image shows cystic implant (arrow) over small bowel loops appearing hypodense due to the internal fluid component. D: Intraoperative image of cystic implants (circle). E: Axial contrast-enhanced CT image shows 4-cm implant of peritoneal carcinomatosis (arrow) presenting as an ovular shape and a mixed structure consisting of a mucinous cystic component and a solid irregular rounded wall showing contrast enhancement. F: Intraoperative image of mixed implants (circle). All images courtesy of Dr. Maria Ciolina and Dr. Andrea Laghi.Peritoneal carcinosis consists of seeding and implantation of neoplastic cells into the peritoneal cavity and may occur in the advanced stages of abdominal and pelvic tumors, but ovarian, stomach, and colorectal cancers account for almost all cases, she explained in the exhibit at ECR 2012. In rare cases, tumors develop directly from the peritoneum (mesothelioma) or extraperitoneal organs (breast cancer). When the disease increases, the tumoral cells reach and affect the membrane covering the same organs (visceral peritoneum).
"Once this barrier has been passed, the affected cells are able to move into the abdominal cavity, carried by the peritoneal fluid. These cells tend to accumulate in those points of greater liquid reabsorption, creating agglomerates that grow more and more, spreading into the whole abdomen and originating the carcinosis," wrote Ciolina, whose team received one of only six Magna Cum Laude awards given by the congress organizers.
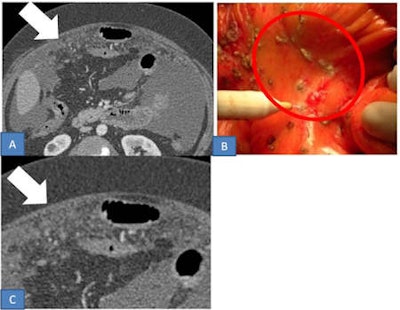 Micronodular pattern in a 60-year-old woman with ovarian cancer. A: Axial contrast-enhanced CT image shows tiny 4-5 mm solid implants (arrow) involving the parietal serous layer. B: Intraoperative image of micronodular implants (circle). C: Magnification of axial CT image.
Micronodular pattern in a 60-year-old woman with ovarian cancer. A: Axial contrast-enhanced CT image shows tiny 4-5 mm solid implants (arrow) involving the parietal serous layer. B: Intraoperative image of micronodular implants (circle). C: Magnification of axial CT image.When neoplastic cells reach the peritoneal cavity, they continue to spread by four possible routes: direct spread along the peritoneal ligaments, mesenteries, and omenta to noncontiguous organs; intraperitoneal seeding via ascitic fluid; lymphatic extension; and embolic hematogenous spread. Intraperitoneal seeding via ascitic fluid is one of the most important ways in which peritoneal metastases spread and is the main cause of peritoneal carcinomatosis, she noted.
Peritoneal carcinomatosis can be thought of as a series of events that together form a peritoneal metastatic cascade, according to medicineworld.org. The peritoneal stromal tissue may be a friendly host for tumor proliferation, providing a rich source of growth factors and chemokines known to be involved in tumor metastasis. Until now, understanding of the molecular mediators that orchestrate this cascade has not been well-understood.
Ciolina wrote that peritoneal carcinosis is characterized by the presence of neoplastic implants with different morphological features and distribution in the peritoneal cavity. Radiologists must evaluate both morphology and localization. Solid, cystic, and mixed implants can present with different patterns that depict typical aspects of peritoneal carcinomatosis.
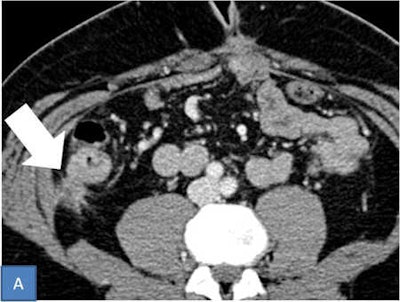 Stellate pattern. Axial contrast-enhanced CT shows a solid nodular implant (arrow) located in right paracolic gutter. That nodule is characterized by spiculated contours providing a stellate pattern.
Stellate pattern. Axial contrast-enhanced CT shows a solid nodular implant (arrow) located in right paracolic gutter. That nodule is characterized by spiculated contours providing a stellate pattern.The micronodular pattern is characterized by the presence of tiny 1- to 5-mm milky spots of peritoneal implants diffusely involving the tunica serosa and subserosal fat. The greater omentum, lesser omentum, and mesentery are typically involved. Conversely, the nodular pattern is characterized by the presence of nodular implants larger than 5 mm diffusely involving the tunica serosa and subserosal fat. Nodules may have an oval shape with rounded contours or a star shape appearance with spiculated margins providing a stellate pattern, she pointed out.
In ovarian carcinomatosis, CT can demonstrate subtle nodularity and stranding of the mesentery and more apparent nodularity along the greater omentum. On the other hand, gastric carcinoma with diffuse gastric wall thickening has a linitis plastica appearance on CT.
"Radiologists must specify every site of peritoneal carcinomatosis in order to provide a staging as detailed as possible," concluded Ciolina. "The best rule to make a good report is to carefully check the surface of the bodies covered by the peritoneal layer, peritoneal ligaments, and peritoneal spaces that surround them."



















