
The nerve disorder trigeminal neuralgia (TN) manifests itself in debilitating paroxysms of facial pain. What causes TN is still a bit of a mystery, but it's commonly attributed to vascular compression of the trigeminal nerve, with an enlarged artery or vein crowding the nerve close to the pons serving as the trigger.
Other possible explanations for TN include nerve atrophy, local lesions, multiple sclerosis, or surgical or dental procedures that result in abnormal or prolonged contact between the vessel and nerve. Whatever the reason, when hyperexcited nerve endings fire, it produces intense shooting pain (American Journal of Roentgenology, December 1994, Vol. 163:6, pp. 1447-1452; Progress in Neurological Surgery, 2007, Vol. 20, pp 235-243).
TN isn't common -- an estimated three to five cases per 100,000 occur annually -- but with the relatively young median age of 67 at diagnosis, it has the potential to be a widespread health issue among aging baby boomers. Initially catching TN can be done clinically so imaging services are not always required.
On the other hand, the options for managing TN are more varied. These range from pharmaceuticals (painkillers or anticonvulsants) to glycerol injection or balloon compression to surgical decompression of the nerve (open surgery, endoscopy).
More recently, radiosurgery has gained popularity as a way to manage TN. But is radiosurgery on its way to becoming the gold standard treatment for TN? While the science on radiosurgery for TN is still being gathered, neurosurgeons who are working with radiosurgery praise it as being just as effective as traditional management methods, but faster and safer.
Finding TN
Except for ruling out dental problems and tumors, imaging has little value in TN assessment, according to the experts. That's mostly because there's generally nothing abnormal (deformation, inflammation) to see on imaging (Radiology, September 1989, Vol. 172:3, pp. 767-770; American Journal of Roentgenology, December 1994, Vol. 163:6, pp. 1447-1452).
"The diagnosis is clinical. There usually is nothing on the MRI scan causing the trigeminal neuralgia, so you make the actual diagnosis from the patient's description of the pain," Dr. George Chovanes, chief of neurosurgery at St. Luke's Hospital in Bethlehem, PA, told AuntMinnie.com.
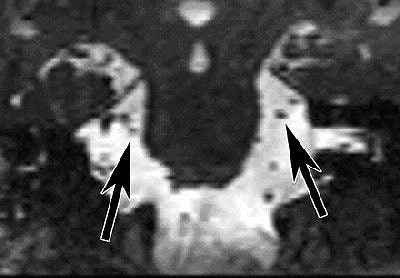 |
| Coronal reformatted image of the brain. Constructive interference in steady state (CISS) MR image (17/8.3) at the level of the ambient cistern reveals trigeminal nerve on right (left arrow) is smaller than trigeminal nerve on left (right arrow). Figure 1, Erbay SH, Bhadelia RA, O'Callaghan M, et al. "Nerve atrophy in severe trigeminal neuralgia: Noninvasive confirmation at MR imaging -- initial experiences." Radiology 2006; 238:689-692. |
Even the most sophisticated imaging exam can't necessarily distinguish between normal and abnormal vessel-nerve contact, according to Dr. Sami Erbay, a neuroradiologist at Lahey Clinic in Burlington, MA, and Tufts-New England Medical Center in Boston.
"The vessel and the nerve can be close to each other and contacting in normal people as well," Erbay said. "That makes it difficult for the imagers to see which one is an innocent contact, and which one is more severe neurovascular compression leading to trigeminal neuralgia."
However, Erbay said that he believes visible TN markers do exist, and he's currently engaged in an ongoing trial to confirm TN with MRI. Erbay and colleagues published some early results of their work last year and found that trigeminal nerve atrophy can be depicted noninvasively with gadolinium-enhanced MRI (Radiology, February 2006, Vol. 238:2, pp. 689-692).
"There are other techniques now coming into clinical use -- one is diffusion tensor imaging -- which track the neurofibers," he said. "If these patients have internal derangements, we may be able to catch that change in the nerve early on with that technique."
Radiosurgical options
Of course, imaging has always played an important part in the surgical planning for TN radiotherapy. Chovanes remembers the early days of pretreatment planning as being quite rudimentary.
"Back in the 1950s, they of course didn't have CT or MRI scans," he said. "Surgical planning was done with radio-opaque enhancement of x-rays, and then they would try to use their crude radiation equipment to hit the nerve. It's only been with the advent of high-speed computerization and excellent imaging that we've been much more successful using radiation to treat trigeminal neuralgia."
These days, planning is done often with CT or MRI, with the latter used for planning and the former for treatment simulation. On the most basic level, all radiosurgery systems deliver high doses of ionizing radiation (65-90 Gy) to small intracranial targets via imaging guidance.
One major difference among radiosurgery systems is the method of patient immobilization. For gamma knife surgery, a cage is bolted to the skull; for linear accelerator-based surgery, a net is fastened to the table.
The gamma knife's cage system "involves numbing up (the patient's) scalp with local anesthetic," Chovanes said. "We put little pins into their skull and hold it in place with a round ring around their head. There's a ring below the eyes and below the face that holds the bars. Once you're clamped into the unit, you can't move your head around at all."
Dr. Kevin Murphy, chief of stereotactic radiosurgery at the University of California, San Diego (UCSD), uses the Trilogy linear accelerator system from Varian Medical Systems of Palo Alto, CA. He describes its frameless head restraint as a mesh and plastic mask that is placed over the patient's face, then fastened to the table, preventing head motion. Other linear accelerator systems also utilize this type of head restraint.
 |
| Proper alignment of patient and assembly is confirmed using lasers. Images courtesy of Dr. Kevin Murphy and University of California, San Diego, department of radiation oncology. |
The type of headgear used for TN treatment makes a big difference. "If you try to bolt someone's head, you can imagine that the V1 (nerve) through the forehead is activated and causes a lot of pain," explained Murphy. "And even if you bolt someone's head, they can still move. Any small muscle relaxation can drop that center off by 2 mm."
The technologies break down into three types:
- Cobalt (gamma knife)
- Linear accelerator (linac)
- Particle beam (proton)
Gamma knife
Gamma knife systems use cobalt-based technology with 201 separate gamma-ray beams that intersect on the target. Invented in the 1950s, it is designed specifically for head and brain surgery. Elekta of Stockholm, Sweden, the manufacturer of Leksell Gamma Knife systems, calculated that 35,000 patients worldwide undergo gamma knife surgery on an annual basis.
But research on gamma knife radiosurgery for TN is still limited. The technique has been used for TN for less than a decade, and trials require follow-up of months to years.
Results of a study from the Roswell Park Cancer Institute in Buffalo, NY, found that at 24 months after radiosurgery, 50% of subjects had poor pain relief and 37% had radiation dose-related facial numbness (Journal of Neurosurgery, March 2005, Vol. 102:3, pp. 442-449).
On the other hand, at Semmelweis University in Budapest, Hungary, neurosurgeons reported that 73% of gamma knife subjects had excellent initial pain relief, 74% had satisfactory pain reduction after 42 months, and 14% were retreated for relapse. While the pain control rate was greater than 70%, 80% of the patients still reported facial numbness (Progress in Neurological Surgery, 2007, Vol. 20, pp 235-243).
Linac
Linac radiosurgery produces a single x-ray beam, rotated to produce multiple intersecting beams. Linac units are starting to see more widespread acceptance, partly because whole-body imaging can be done on them.
In a 2004 report, radiation oncologists from the University of Minnesota-Twin Cities in Minneapolis said that 35% of their TN patients treated with linac had complete pain relief. Sixty-three percent had pain recurrence in a mean period of 21.5 months, and 43% reported a 50% or more decrease in pain severity (Stereotactic and Functional Neurosurgery, 2004, Vol. 82:5-6, pp. 244-249).
In a 2005 study, 57% of TN patients treated with linac achieved complete pain relief, while 75% experienced pain reduction. The median time to pain relief was one month, stated the researchers from the University of Wisconsin Medical School in Madison (Neurosurgery, December 2005, Vol. 57:6, pp. 1193-1200).
Proton
Finally, proton systems, which use three to five fixed beams of protons, neutrons, or helium ions, are currently under investigation, mostly for cancer treatment. According to a recent report in Technology in Cancer Research & Treatment, four hospitals and one clinic in the U.S. and five other facilities in Japan offer proton treatment.
"The accelerator types are a combination of synchrotrons, cyclotrons, and linear accelerators; some carry advanced features such as respiration gating, intensity modulation, and rapid energy changes, which contribute to better dose conformity on the tumor when using heavy charged particles," explained a group from Loma Linda University Medical Center in Loma Linda, CA (Technology in Cancer Research & Treatment, August 2007, Vol. 6:4 supplement, pp. 49-54).
In January 2007, Varian Medical Systems acquired a supplier of proton therapy systems. In September, the company introduced its spot-scanning proton therapy technology at the 2007 European Society for Therapeutic Radiology and Oncology (ESTRO) meeting in Barcelona, Spain.
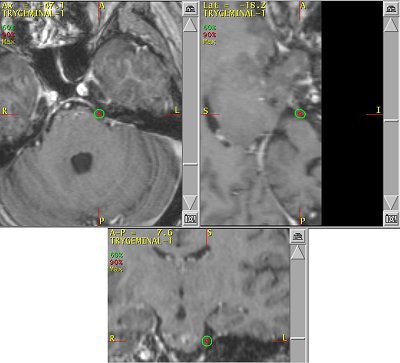 |
| An example of a treatment plan for TN using a single isocenter to deliver a single fraction of 80 Gy to the TN nerve root. A single 5-mm collimator and a multiarc technique would be used to minimize dose to the brain stem. Image courtesy of Varian Medical Systems, Palo Alto, CA. |
Meanwhile, BrainLab of Feldkirchen, Germany, has a system that uses high-dose photon energy, which is shaped by the tumor contours. According to an early report by radiation oncologists at the Centre Hospitalier Universitaire Vaudois in Lausanne, Switzerland, their experience with 17 TN patients treated with the system was a positive one. Thirty-five percent of the patients reported complete pain relief, while the remainder reported occasional or partial relief. The investigators found no major complications (Swiss Medical Weekly, December 1, 2007, Vol. 137:47-48, pp. 682-686).
What users say
To understand how TN radiosurgery is succeeding in the real world, it's best to talk to people who use it. For the most part, experts rely on both linac and gamma knife systems.
According to Accuray of Sunnyvale, CA, its CyberKnife system (below) has been used on 35,000 patients worldwide. Dr. Richard Bucholz, a neurosurgeon at St. Louis University Hospital in Missouri told AuntMinnie.com, "We've had our (CyberKnife system) for about three years. We're up to about 65 TN patients on it. So far, we've been extremely happy. Our relapse incidence is about 3% to 5%."
 |
| The CyberKnife system. Image courtesy of Accuray, Sunnyvale, CA. |
Dr. John Adler, a professor of neurosurgery at Stanford University Medical Center in Stanford, CA, said his group has performed 120 TN linac surgeries (100 with CyberKnife) to date. "For five-plus years we have been lesioning an elongated segment of trigeminal nerve with the CyberKnife; this is in contrast to the gamma knife's 4-mm spherical lesion," he said. Adler added that the procedure has provided long-term (more than three to four years) pain relief in most patients, with a relapse rate of less than 5%. An initial 75% incidence of facial numbness has since decreased.
"Over the past three years, and following a significant dose/volume de-escalation, the risk of facial numbness has been reduced to about 15%. Since beginning the simultaneous use of a radiation scavenger, amifostine, one year ago, I have had no cases of facial numbness," he said.
St. Luke's has used both a gamma knife system and Varian's Trilogy linac system for TN treatment, but now does all its radiosurgery with its 1-year-old Trilogy system.
One reason for the switch, Chovanes said, was that "you can deliver the energy quicker (with Trilogy). With the gamma knife, you have these fixed cobalt sources, which gradually run down. As the years go by, you have to keep the patient in the unit longer and longer to allow the proper energy to be delivered." However, he said he did still prefer the gamma knife-style bolt-on headgear.
Murphy and colleagues at UCSD work with a linac system (Trilogy) and also perform gamma knife surgery. Time is one major difference between the two options in TN. A procedure with the Trilogy system takes about 30 to 40 minutes versus about two to three hours with the gamma knife, he said.
 |
| Same patient as above. CT scan is obtained in treatment position (FOV 35 cm, 1.25-mm slice thickness, no contrast). Images courtesy of Dr. Kevin Murphy and University of California, San Diego, department of radiation oncology. |
Again, the type of head restraint makes a difference. Trilogy's mesh mask can be used with a dental bite tray that has "little fiducial markers that an infrared camera can 'talk' to," Murphy said. "It's been around in (operating rooms) for a while" for position monitoring, he added.
UCSD started treating TN with the Trilogy system about a year ago, performing one to two procedures on a monthly basis. Initially, they reserved linac-based surgery for TN patients when other surgeries had failed, he said.
"We treated three patients who didn't want further gamma knife procedures with the bolted headframe. So far, all three are pain-free and they're very happy. Usually in a week to a month their pain goes away," he said.
Murphy's list of linac shortcomings is, well, short. "I trained on (gamma knife). To train on a (Trilogy) system that was frameless and not proven was a hard thing to do. The dose is really high (90 Gy, four times the regular radiotherapy dose, but the same as gamma knife), and it's right next to the brain stem, so if you miss or the patient moves, you're going to fry the brain stem," he said.
To be on the safe side, Murphy said he aims the radiation about a centimeter downstream from the target (away from the brain stem) and does redundant positioning verification.
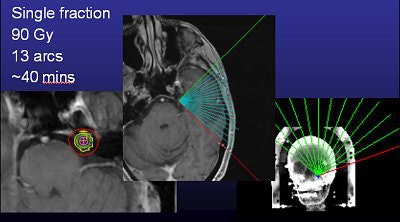 |
| Above, frameless radiosurgery for TN. Below, three months after treatment. Images courtesy of Dr. Kevin Murphy and the University of California, San Diego, department of radiation oncology. |
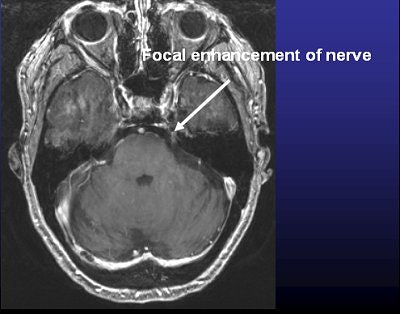 |
Some TN treatment centers still prefer to stick with gamma knife surgery. "Over the years we've shifted trigeminal neuralgia treatment to gamma knife treatment," said Erbay. "Tufts-New England Medical Center hosts the only (gamma knife) treatment center in the state of Massachusetts."
Kathy Garizio, outreach coordinator for Long Island Gamma Knife in Oceanside, NY, is a former gamma knife nurse who is a tireless champion of the technique -- bolts and all. She pointed out that gamma knife is specialized for use in the head, making it more precise.
"The biggest thing is the accuracy. In the brain, there's no room for error," she said. In addition, while head nets may appeal more to patients, linac masks "actually lock on the table, so the patient can't move."
Will radiosurgery become the gold standard for treating TN? The research is still ongoing. A 2006 study compared microvascular decompression (MVD) to gamma knife surgery and found that the average patient self-rated satisfaction score, based on a 10-point scale, with gamma knife treatment was 6.4 versus 8.7 for MVD (Journal of Clinical Neuroscience, February 2006, Vol. 13:2, pp. 239-244).
In another study, a group at Cooper University Medical Center in Camden, NJ, concluded that percutaneous retrogasserian glycerol rhizotomy was a better bet in TN patients requiring urgent pain relief, while gamma knife surgery should be reserved for patients who are unsuitable candidates for MVD (International Journal of Radiation Oncology, Biology, Physics, September 1, 2005, Vol. 63:1, pp. 82-89).
Unfortunately, no studies to date have compared patient outcomes using different radiosurgery techniques, according to Murphy.
At institutions where radiosurgery is available, it's becoming the first-line treatment for pharmacologically resistant TN. But whether radiosurgery will become the gold standard for treating all TN is still up for discussion. Adler said he believes it's the gold standard, but also warned that TN radiosurgery needs to continue to prove itself in peer-reviewed literature.
Murphy said he is optimistic about the future of TN radiosurgery, especially as the advancements are made in the area of the headframes. "This procedure appears to beautifully address a subset of patients that cannot or do not want to undergo surgery," he said.
By Sydney Schuster
AuntMinnie.com contributing writer
December 31, 2007
Related Reading
Stereotactic radiosurgery improves survival after melanoma brain metastases, May 24, 2007
New study questions benefit of trigeminal radiosurgery for cluster headache, February 7, 2005
Radiosurgery shows promise as primary treatment for trigeminal neuralgia, March 3, 2004
Copyright © 2007 AuntMinnie.com


















