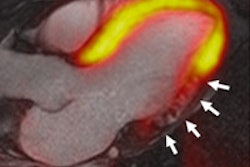
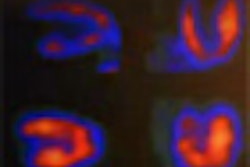
Myocardial perfusion abnormalities obtained after stress, as well as the extent of scar tissue detected by gated SPECT, are the best predictors of cardiac events in patients with suspected or known ischemic heart disease.
That conclusion comes from Italian researchers, who also found that gated SPECT outperforms extensive diagnostic workups and coronary arteriography to predict cardiac event-free survival, which, in turn, will prompt preventive therapies that may benefit patient health.
The findings were published in the April 2009 issue of the Journal of Nuclear Medicine (Vol. 50, pp. 546-553), with Dr. Alessia Gimelli from the G. Monasterio Foundation in Pisa as the lead author.
Researchers at the foundation's CNR Clinical Physiology Institute selected a group of consecutive patients from their database that dates back to 2000. The patients had known or suspected ischemic heart disease and had undergone a complete diagnostic workup that included stress and rest myocardial perfusion imaging and coronary arteriography.
The study excluded patients with acute or recent myocardial infarction, previous coronary artery bypass graft surgery, chronic renal failure under dialysis treatment, or primary overt hyperthyroidism.
Patient population
A total of 539 patients between the ages of 55 and 75 underwent exercise stress testing, while 137 patients were given a dipyridamole stress test. Of the 539 patients undergoing the stress test, 387 subjects reached 85% of the maximal predicted heart rate, 58 patients reached from 80% to 85% of the maximal predicted heart rate, and the remaining 94 patients did not reach the target heart rate and were injected for significant ST segment depression or ventricular arrhythmias.
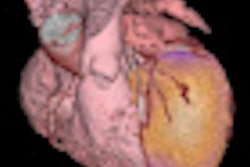
The diagnostic workup included clinical evaluation, laboratory tests, electrocardiography, 2D echocardiography, stress and rest gated SPECT, and coronary arteriography to diagnose ischemic heart disease. Gated SPECT was performed before coronary arteriography in 623 patients (92%) and after arteriography in the remaining 53 patients (8%).
Gated SPECT was performed with dual-head gamma cameras (e.cam, Siemens Healthcare, Erlangen, Germany; Millennium MC, GE Healthcare, Chalfont St. Giles, U.K.) equipped with high-resolution collimators.
Follow-up data
Over 37 months, the researchers followed patients as they returned for periodic examinations. From those results, the researchers determined that gated SPECT was the best predictor of future cardiac events, compared with left ventricular ejection fraction, coronary arteriography, laboratory tests, and other measures.
Of the 492 patients with confirmed ischemic heart disease, 187 patients were treated medically for the condition, and 305 patients were revascularized by percutaneous coronary interventions (180 patients), coronary artery bypass graft surgery (110 patients), or both procedures (15 patients). Medically managed patients had a lower number coronary vessels affected by stenosis than patients who received revascularizations.
The study credited improved techniques in nuclear cardiology for assessing the clinical profile of patients with ischemic heart disease, who today are older and affected by more diseases than in the past. "We were ... surprised to see that gated SPECT remains the best predictor of future cardiac events in patients with ischemic heart disease," the researchers noted.
Regarding left ventricular ejection fraction, SPECT images were superior in showing the extent of damage to the heart muscle and, thus, a better predictor of patient outcome. The researchers noted that one of the benefits of SPECT's ability to identify individuals at risk for future cardiac events is that it can prompt earlier intervention with therapies that may alter the course of the disease.
As for limitations, the study noted that the patient sample has "an intermediate pretest probability" of coronary artery disease that does not reflect the general population undergoing gated SPECT for known or suspected ischemic heart disease.
It's likely that the enrolled patients, the authors write, "reflect a higher-risk population, as indirectly shown by the high prevalence of previous myocardial infarction (43%) and the main cardiovascular risk factors, and by the fact that all enrolled patients underwent coronary arteriography."
By Wayne Forrest
AuntMinnie.com staff writer
April 13, 2009
Related Reading
ACC study: Most cardiac SPECT scans are appropriate, April 1, 2009
MRI, MDCT err in estimating cardiac functional parameters, February 20, 2009
Hybrid 3D echo/SPECT technique produces better CAD imaging, February 12, 2009
SPECT MPI predicts sudden cardiac death, September 26, 2008
PET, SPECT measures of LVEF have superior predictive value, March 13, 2006
Copyright © 2009 AuntMinnie.com