A large study of patients who developed contralateral lung cancer after having a pneumonectomy suggests that stereotactic radiation therapy is a curative option with minimal toxicity, even for high-risk patients with chronic obstructive pulmonary disease.
A small percentage of patients who survive cancer in one lung will have recurrence of a primary cancer tumor in the other lung, with the risk increasing the more years these individuals survive. A high risk of complications can rule out surgery for patients who have already had one lung removed. However, stereotactic radiation therapy is proving to be an effective alternative.
Researchers at Vrije University Medical Center in Amsterdam, the Netherlands, reported the clinical outcomes of postpneumonectomy patients who had been treated with stereotactic radiation therapy at the facility and at Catharina Hospital in Eindhoven. They published their results online on January 6 in Cancer.
Since 2003, a total of 15 patients who developed a second lung tumor in the contralateral lung received stereotactic radiation therapy at the cancer centers. Eleven patients had pneumonectomies as the initial surgical treatment and four had lobectomies. The second cancers occurred between 10 months and 29 years after completion of the first lung cancer treatment, with a median interval of 8.9 years.
The patients represented all categories of chronic obstructive pulmonary disease: three patients had no disease, one patient had mild disease, four patients had moderate disease, five patients had severe disease, and two patients had very severe disease. Because bronchoscopy would be a high-risk diagnostic procedure for most of these patients, diagnosis was made by a multidisciplinary tumor board analyzing FDG-PET images showing a positive lesion with radiological characteristics of malignancy.
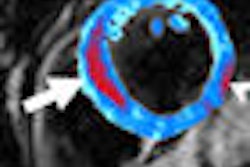
Stereotactic radiation therapy was planned and delivered using eight to 11 radiation beams and respiration-correlated 4D CT scans to account for tumor motion, according to lead author Dr. Cornelis Haasbeek, a radiation oncologist at Vrije University Medical Center. Treatment was delivered without interruption to all patients between seven and 20 days.
The planning target volume consisted of the tumor volume, including all respiratory motion derived from the 4D CT scan, plus an additional safety margin of 3 mm.
All doses were prescribed to the 80% isodose level (range, 99.3%-100%), and treatment plans were optimized to achieve highly conformal irradiation and to minimize the dose to the remaining lung, the thoracic wall, mediastinal structures, and the spinal cord. Also, risk-adapted dose schemes (from 3 x 20 Gy to 8 x 7.5 Gy) were used, depending upon tumor size, location, and partial overlap with prior radiotherapy fields.
Orthogonal x-ray imaging devices integrated in the linear accelerator or by using conebeam CT were used to check patient position and to make corrections before each treatment fraction. All schedules for the patients were equivalent to a biologically effective dose ranging from 105 to 180 Gy to achieve very high local control. Lung doses were evaluated by calculating a value termed V20, the percentage of lung that received a total radiation dose greater than or equal to 20 Gy.
After treatment, all patients were followed prospectively by serial CT scans and quality-of-life measurements at three months, six months, and 12 months, and yearly thereafter.
During the follow-up period, which ranged from four months to 55 months (median, 16.5 months), one patient died. This patient developed widespread bony metastasis eight months after treatment. The researchers also reported that one patient underwent palliative chemotherapy for an isolated mediastinal lymph node failure.
Early toxicity was limited to mild fatigue in four patients, and two patients developed episodes of late grade 3 toxicity, from which both recovered. In 2008, 14 patients remained alive and disease-free.
Because stereotactic radiation therapy now offers an effective and low-risk treatment, the authors strongly suggested that surveillance be initiated for these patients, and that clinical guidelines be modified to recommend screening programs for patients with pneumonectomies.
By Cynthia E. Keen
AuntMinnie.com staff writer
February 13, 2009
Related Reading
Stereotactic single-dose radiotherapy an option for early lung cancer, August 29, 2007
Incidentally detected lung cancers less likely to require pneumonectomy, February 5, 2007
Copyright © 2009 AuntMinnie.com