PET/CT with the radiopharmaceutical gallium-68 (Ga-68) prostate-specific membrane antigen (PSMA) should be the choice over whole-body-MRI for detecting prostate cancer recurrence after radical prostatectomy, a German group advocates in a study published by the European Journal of Nuclear Medicine and Molecular Imaging.
 Dr. Lino Sawicki from the University of Düsseldorf.
Dr. Lino Sawicki from the University of Düsseldorf.Ga-68 PSMA PET/CT achieved a statistically significant superiority in a direct comparison with whole-body MRI both on a per-lesion and a per-patient basis. Ga-68 PSMA PET/CT discovered cancer recurrence in more patients, and it also found more lesions than its imaging counterpart (EJNMMI, March 16, 2019).
"Our results underscore the excellent performance of Ga-68 PSMA PET/CT for whole-body staging of prostate cancer patients with biochemical recurrence after radical prostatectomy," wrote lead author Dr. Lino Sawicki and colleagues from the University of Düsseldorf. "Whole-body MRI provides a significantly lower lesion detection rate and inferior diagnostic confidence compared with Ga-68 PSMA PET/CT ... [and] carries a considerable risk of missing small lymph node metastases."
Prostate cancer assessment
Since its clinical inception in 2013, Ga-68 PSMA PET/CT has quickly become the gold standard for prostate cancer primary staging and restaging, and it has been endorsed for imaging in men with biochemical recurrence after radical prostatectomy. Based on previous studies, Ga-68 PSMA PET/CT has shown the ability to identify pathological prostate cancer lesion uptake in patients with prostate-specific antigen (PSA) levels as low as 2 ng/mL or less. The technique also achieves better diagnostic accuracy than PET imaging with F-18 choline or C-11 acetate.
On the other hand, Ga-68 PSMA PET/CT can result in false-negative results "due to low PSMA expression (about 5% of prostate cancer) or masking of prostate cancer lesions in or adjacent to organs with high background activity," the authors noted.
MRI also has come to the forefront in recent years as a useful modality for detecting prostate cancer recurrence. Its soft-tissue contrast and diffusion-weighted MR imaging (DWI-MRI) protocol have found disease recurrence among patients with altered pelvic anatomy following radical prostatectomy.
"However, with regard to the diagnostic performance of whole-body MRI compared to Ga-68 PSMA PET/CT, the few studies that are available did not focus on patients with disease relapse," the German researchers wrote. "Hence, the purpose of this study was to prospectively compare the diagnostic performance of whole-body MRI with that of Ga-68 PSMA PET/CT for the detection of biochemical recurrence in prostate cancer patients."
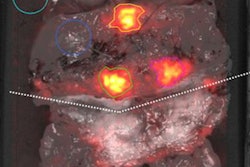
In fact, Sawicki and colleagues are well-versed in the utility of Ga-68 PSMA to assess cancer cases. Their 2017 study combined the radiopharmaceutical with PET/MRI to better detect and classify local lesions and distant metastases in women suspected of having recurrent pelvic cancer than MRI alone. They went on to advocate that the hybrid modality be considered a valuable alternative for whole-body staging of patients with suspected recurrent disease.
In the current study, the researchers prospectively enrolled 28 consecutive male patients (mean age, 65.3 ± 9.0 years) with newly confirmed cases of prostate cancer recurrence (PSA ≥ 0.2 ng/mL) who had undergone radical prostatectomy. All the patients underwent both whole-body 1.5-tesla MRI scans (Magnetom Avanto, Siemens Healthineers) with a dedicated pelvic imaging protocol and Ga-68 PSMA PET/CT scans (Biograph mCT 128, Siemens). PET/CT was performed one hour after intravenous injection of Ga-68 PSMA (mean, 166 ± 35 MBq). The scans took place within a limited time of 11 (± 10) days. The average PSA level in the patients at the time of imaging was 2.09 (± 1.95) ng/mL (range, 0.2-9.9 ng/mL).
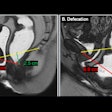
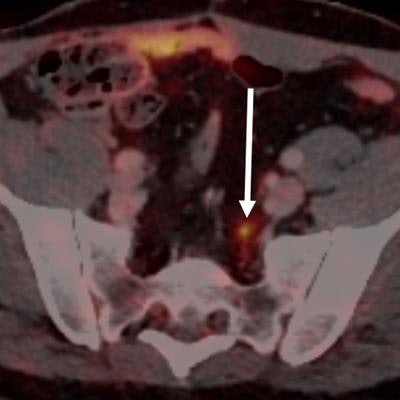
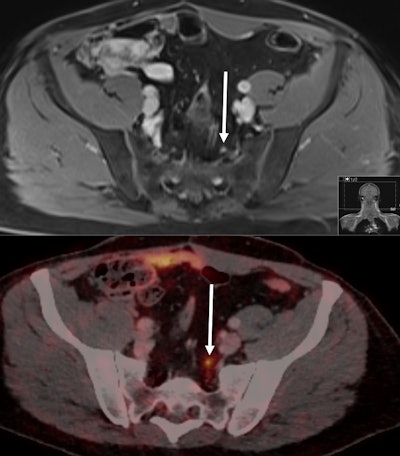 Images from a 55-year-old patient with biochemical recurrence of prostate cancer following radical prostatectomy four years previously. His PSA rose to 0.51 ng/mL at the time of imaging. PSMA-PET CT (bottom) identified a 5-mm small lymph node metastasis due to the pathologic PSMA uptake in the left presacral region (maximum standardized update value of 6.1). The lymph node was falsely rated as nonmalignant on MRI based on its small size and ovoid shape. Images courtesy of Sawicki et al.
Images from a 55-year-old patient with biochemical recurrence of prostate cancer following radical prostatectomy four years previously. His PSA rose to 0.51 ng/mL at the time of imaging. PSMA-PET CT (bottom) identified a 5-mm small lymph node metastasis due to the pathologic PSMA uptake in the left presacral region (maximum standardized update value of 6.1). The lymph node was falsely rated as nonmalignant on MRI based on its small size and ovoid shape. Images courtesy of Sawicki et al.Head-to-head comparison
Ga-68 PSMA PET/CT detected prostate cancer lesions in 20 of the 28 patients (71%) with disease recurrence, compared with MRI's detection of prostate cancer lesions in 11 patients (39%) with recurrence. The difference between the two modalities in this per-patient comparison was statistically significant (p = 0.0167).
Interestingly, Ga-68 PSMA PET/CT and whole-body MRI detected prostate cancer lesions in the same 11 patients and missed prostate cancer relapse in the same eight patients. The difference was that Ga-68 PSMA PET/CT discovered lesions in nine additional patients.
Among the 20 patients with disease recurrence, there were a total of 56 prostate cancer lesions. Ga-68 PSMA PET/CT found all 56 of them (100%), compared with whole-body MRI, which detected only 13 prostate cancer lesions (23%), missing 43 (77%) lesions. Again the difference in performance was statistically significant (p < 0.001), and there were no false-positive findings among either modality, according to the researchers.
"The superior diagnostic confidence of 68Ga-PSMA PET/CT reflects another beneficial feature of hybrid imaging: It reduces ambiguity in lesion assessment in comparison with conventional imaging," they added.
Given the disparity in the results, the overall diagnostic confidence of Ga-68 PSMA PET/CT (2.7 ± 0.7) to characterize prostate cancer lesions was predictably and significantly greater than whole-body MRI (2.3 ± 0.6) (p = 0.044).
"The results of our study demonstrate a higher tumor detection rate in patients with biochemical recurrence of prostate cancer with Ga-68 PSMA PET/CT than with whole-body MRI," Sawicki and colleagues concluded. "Ga-68 PSMA PET/CT was superior on a per-patient basis, allowing localization of relapse in significantly more patients than whole-body MRI. Additionally, Ga-68 PSMA PET/CT provided better diagnostic confidence than whole-body MRI."