As hybrid imaging gains more ground in cardiology, neurology, and oncology, the debate over PET/MRI's current and potential role in routine practice still rages. The central question remains: Is it an expensive new toy with no clinical applications on the horizon, or is it a truly revolutionary technique?
Both subspecialists and generalists attending today's E3 418 session on Scanners and Tracers -- the first of a six-part course with the more advanced sessions scheduled for Friday and Saturday -- will learn about the latest on hybrid imaging's current role, and also about new developments, particularly in tracers. In addition, they will hear how erratic reimbursement for procedures across Europe is slowing the mass adoption of these promising tools, throwing their long-term future into doubt. To help counter this, one expert proposes a new generation of subspecialist: the hybrid imaging physician.
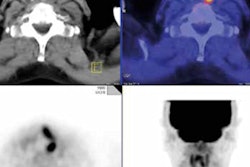
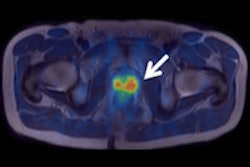
 Images show carcinoma at the esophagogastric junction before therapy (pre therapy) and after two cycles of chemotherapy (post therapy). The image after two cycles of chemotherapy demonstrates complete metabolic response. Image courtesy of Dr. Gerald Antoch.
Images show carcinoma at the esophagogastric junction before therapy (pre therapy) and after two cycles of chemotherapy (post therapy). The image after two cycles of chemotherapy demonstrates complete metabolic response. Image courtesy of Dr. Gerald Antoch.Understanding the technical basics of hybrid imaging is vital for doctors keen to avoid the trap of misinterpreting artefacts as pathological findings. Specifically, attendees at today's basic session will discover how morphological and functional imaging interact and how this interaction may lead to false positives or lower quality pictures, according to moderator Dr. Gerald Antoch, chair of radiology at Düsseldorf University Hospital in Germany.
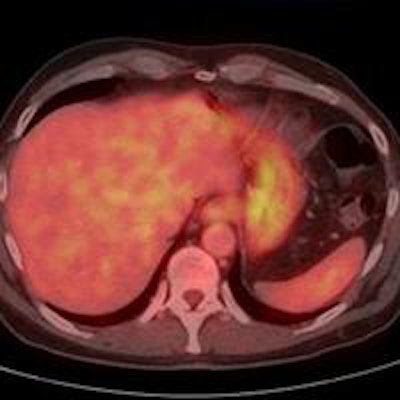
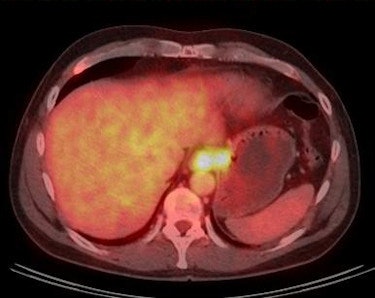
"Accurate hybrid imaging is a question of knowledge. The issue of artifacts arising from patient implants or from CT contrast material used in PET/CT has been thoroughly assessed in the literature. Known to a lesser degree, however, are infrequent artifacts visualized on PET or areas of physiological tracer uptake simulating disease," he said. "Body parts such as the gastrointestinal tract may also focally take up FDG, which may be misinterpreted as a tumor. This will be known to regular hybrid imagers, but not to the general radiologist typically using it once in a while for oncological questions."
 Optimizing workflow and streamlining costs depends on training hybrid imaging specialists, according to Dr. Gerald Antoch, chair of radiology at Düsseldorf University Hospital.
Optimizing workflow and streamlining costs depends on training hybrid imaging specialists, according to Dr. Gerald Antoch, chair of radiology at Düsseldorf University Hospital.The main challenge to hybrid imaging is getting the nuclear medicine physicians and radiologists involved in it together, Antoch explained. At most sites, at least two people are required to generate one report, and this is heavy on resources and time. Speaking to ECR Today ahead of the congress, he underlined the need for the hybrid imager to be a specialist, both in radiology and nuclear medicine, and this is where the hybrid imaging physician fits in.
"In the long run, doctors need to be trained in both disciplines to read hybrid datasets autonomously. However, in the present system, the hybrid imager has to be certified by both radiology and nuclear medicine boards. In Germany, certification per board requires five years of training, and two board certifications nearly double the time," he noted.
One idea that might be politically problematic is a common imaging trunk of two years and then specialization in hybrid imaging, general radiology, or general nuclear medicine. When enough people have eventually been trained in both radiology and nuclear medicine, these hybrid imaging physicians could read datasets by themselves, Antoch continued.
For now, while in smaller centers one reader may have both certificates, in larger institutes the report is often written by a resident from the radiology or nuclear medicine department, and then later verified by a board certified radiologist and a board certified nuclear medicine physician.
"We may only be able to supply such manpower in big university hospitals. However, time constraints and issues of affordability have and will become more important. Thus, optimizing workflow by training hybrid imaging specialists must be considered an important goal for the future," he said.
The future of hybrid imaging is to some extent dependent on reimbursement, which in some countries remains limited, while other member states enjoy a more liberal and evidence-based reimbursement policy.
"If not reimbursed, it will be difficult for hybrid imaging to evolve as doctors won't use it. Although it is already implemented in clinical routine, further use depends on country-specific policies," Antoch said.
Echoing his sentiments, Thomas Beyer, PhD, professor of the physics of medical imaging at the Medical University of Vienna, looks forward to the panel discussion in which ideas on how costs and reimbursement are likely to affect hybrid procedure use will be floated. Reimbursement of PET is not adequate, according to Beyer, who pointed to zero reimbursement in Austria, compared with reimbursement for two indications in Germany and for almost all indications in Switzerland.
_Beyer.png?auto=format%2Ccompress&fit=max&q=70&w=400) The future of PET/MRI will be ensured only by defining its key clinical applications and resolving reimbursement issues and developing new tracers, according to Thomas Beyer, PhD, professor of the Physics of Medical Imaging, Medical University of Vienna.
The future of PET/MRI will be ensured only by defining its key clinical applications and resolving reimbursement issues and developing new tracers, according to Thomas Beyer, PhD, professor of the Physics of Medical Imaging, Medical University of Vienna.His own talk is to focus on what systems are available and how they work.
Fully integrated PET/CT, the main workhorse of hybrid imaging, accounts for about 10% of all CT production, with 5,000 units operational worldwide today, and with 95% of use dedicated to initial staging and restaging oncology questions as well as therapy response, 3% used for neuro-oncology, and 2% for cardiology questions.
Three years since the commercial introduction of PET/MRI, there are still only around 60 units installed worldwide.
"So far there has been no hard evidence to support the diagnostic benefit of PET/MR, which begs the question of why doctors perform it," Beyer told ECR Today.
He suggests part of the answer lies in MR's capacity to yield more information than CT, particularly due to its better soft-tissue contrast and ability to visualize selected aspects of physiological and molecular pathways. Simultaneous PET/MR also allows doctors to follow tracer distributions over time and combine quantitative molecular PET information with information on cellular densities, flow, and perfusion, such as data obtained from advanced MR-based spectroscopy, diffusion, and perfusion studies.
"Such a simultaneous and synergistic approach generates more useful information than consecutive imaging. The big question now is: Will research lead to new clinical applications adopted into the workflow?" he noted.
Applications, and therefore the future of hybrid, will be defined by the availability of molecular tracers. New tracers that become very specific, thus providing very little anatomical background information but very high sensitivity and specificity, will promote the use of hybrid imaging, and PET/MR in particular.
SPECT/CT is likely to become increasingly organ-specific, with the use of cadmium zinc telluride (CZT) solid state detectors, according to Beyer. Advances in data handling, image processing, and reconstruction will yield quantitative data, similar to those acquired in PET.
"The future of PET/MR is linked to finding its key application. I suspect that this will be in neurodegenerative disease," he said. "Pediatric oncology is also an area where PET/MR promises much because MRI can provide good image contrast with little body fat typically found in children."
Multiparametric imaging using MRI and PET/CT will also continue to be investigated, and may increasingly yield answers to clinical questions.
"All three combinations of hybrid imaging -- PET/CT, SPECT/CT, and PET/MR -- are at a technological state where they can be used clinically, but this mandates a multidisciplinary approach," Beyer summed up. "Technology has provided the tools; now it's down to the humans to make the best of them."
Originally published in ECR Today on 4 March 2015.
Copyright © 2015 European Society of Radiology