As the cost-effectiveness of colorectal cancer screening comes under growing scrutiny across Europe, detailed, up-to-date analysis and statistics involving more than 1,100 patients recruited into the Dutch population-based screening trial look certain to attract widespread attention.
Average costs per participant within the Dutch program was 169.4 euros, and average CT colonography (CTC) costs per individual with detected advanced neoplasia were 2,772.5 euros, according to lead researcher Dr. Margriet de Haan, PhD, from the department of radiology at Academic Medical Center in Amsterdam. The unit costs per CTC (from intake to communication of results) were 144 euros for participants with a negative result and 153 euros for those with a positive result.
In the sensitivity analyses, the unit costs were predominantly influenced by anticipated higher costs for post-CTC consultation by the general practitioner, closely followed by the effect of changes in the average number of CTCs per hour. By increasing the number of CTCs per hour, the costs per CTC could be decreased substantially.
In light of the findings, previous cost-effectiveness analyses should probably be updated, de Haan and colleagues noted in an article published online on 9 November by European Radiology.
"We found that the actual unit costs per CT colonography when used in a dedicated primary screening setting were, at least in the Netherlands, substantially lower compared with the estimated unit costs that were used in previous cost-effectiveness analyses, which were usually based on reimbursement rates in the clinical situation," de Haan and colleagues wrote. "This warrants the need of reconsidering cost-effectiveness, at least for the Dutch situation."
Between June 2009 and August 2010, 2,920 patients were invited for CTC screening. Of these, 1,134 (38.8%) were willing to participate. After the intake, 47 respondents were excluded (34 with full-bowel examinations in previous five years, 10 with life expectancy of less than five years, one with inflammatory bowel disease, two with hyperthyroidism), and the remaining 1,087 (37.2%) were scheduled for CTC. After making the appointment, 105 participants dropped out, leaving 982 patients (33.6%). In 44 participants, the quality of the CTC was insufficient, 33 participants underwent a re-examination (1.1% of invitees), and 11 refused.
Of the invitees, 47.2% were reminded, 38.8% scheduled for an intake, 37.2% scheduled for CTC, 33.6% underwent CTC, and 1.1% needed a re-examination. Lesions greater than 10 mm in diameter were detected in 2.9% of the invitees. Invitation costs were 5.6 euros. Costs per CTC (intake to results) were 144 euros. Extra costs of communication of positive results were 9 euros. Average costs of invitational-based CTC screening were 57 euros per invitee, 169.4 euros per participant, and 2,772.5 euros per individual with detected advanced neoplasia, the authors stated.
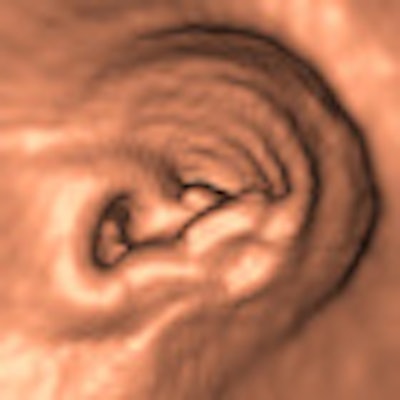
Participants received a noncathartic bowel preparation consisting of three 50-mL doses of iodinated contrast agent (Telebrix Gastro, Guerbet), combined with a low-fiber diet for a day. The CTC examinations were performed in two screening centers by experienced personnel using 64-slice CT (Brilliance, Philips Healthcare) with a low-dose protocol with 25 ref mAs and slice thickness of 0.9 mm. Colonic distension was obtained with an automatic CO2 insufflator (ProtoCO2l, Bracco Diagnostics) after intravenous administration of 20 mg of hyoscine butylbromide (Buscopan, Boehringer Ingelheim).
All CTC scans were read within two weeks after the procedure by one experienced radiologist (≥ 800 examinations), using primary 2D read (window setting 1500, -250 HU) with 3D problem solving using 3D visualization software (unfolded view, View Forum; Philips), followed by secondary CAD read. All detected intracolonic lesions 6 mm and larger were reported. A nurse or physician informed the screenee by telephone about the final CTC result. In addition, the general practitioner and the screenee received a result letter by mail, which was sent by the screening organization.
The study showed that a substantial decrease in costs can be realized by including expected bulk discounts in the model. The unit costs per invitee were 57 euros (range 46.76 to 56.51; worst-case versus best-case scenario). The unit costs per participant were 169.4 euros (range 128.43 to 194.83; best-case versus worst-case scenario).
An advantage of the study was that data were collected on the estimated unit costs for CTC screening in a population-based colorectal cancer screening trial, according to the authors. Costs for CTC in a high-risk population would probably have overestimated the procedural costs as these patients are usually symptomatic, as well as more fragile and older relative to screening invitees, leading to increased performance times and increased costs per CTC. In the design of the logistics of this study, they aimed to perform the invitation procedure and procedure itself as efficiently as possible.
It is questionable whether these results can be generalized to other hospitals and other countries, the researchers wrote. The data were derived in a university hospital, which may lead to an overestimation or underestimation of the costs compared with smaller hospitals. Also, the costs were based on Dutch rates for CT machines and material costs, as well as the organization of the Dutch healthcare system. The estimated costs of important parts of the entire screening procedure, such as performing an intake, evaluation of the CTC, and communication of the results, are predominantly defined by personnel costs, which will vary from country to country. Furthermore, the authors were not able to specify the personnel costs and overhead costs that were made by the screening organizations.
Overall, however, the cost estimate of performing similar CTC screening can be adapted to other settings by providing details of the screening procedure and its cost structure, they concluded.