Overriding evidence of CT colonography's cost-effectiveness remains absent, the main problem being that most studies have different comparators and parameter values, according to new analysis by Irish researchers.
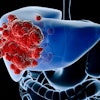
Colorectal cancer is the most common cancer diagnosed in Europe, and the European Code Against Cancer recommends individuals 50 and older get screened for it. There are two kinds of screening tests: stool-based test (such as fecal occult blood tests [FOBT], fecal immunochemical tests [FIT], and fecal DNA tests) and structural colon tests (rigid and flexible sigmoidoscopy [FS], colonoscopy, and CT colonography [CTC]). The optimal test is unclear, but CTC is certainly a contender, noted Paul Hanly, PhD, a health economist from the National Cancer Registry, Ireland in Cork, and his co-authors, who included Dr. Helen Fenlon, a radiologist at Dublin's Mater Misericordiae University Hospital (International Journal of Technology Assessment in Health Care, October 2012, Vol. 28:4, pp. 415-423).
The researchers systematically reviewed the evidence on the cost-effectiveness of CTC as a screening tool with a focus on identifying key factors influencing findings. They searched PubMed, Medline, and the Cochrane Library for cost-effectiveness or cost-utility analyses of CTC-based screening. Sixteen studies were identified from the U.S., Canada, France, Italy, and the U.K. Eleven studies considered direct medical costs only, while five included indirect costs as well. Fourteen studies compared CTC with no screening, 14 compared CTC with colonoscopy-based screening, and fewer studies compared CTC with sigmoidoscopy or fecal tests.
Outcomes assessed were life years gained or saved (13), quality-assisted life years (2), or both (1). Three studies considered extracolonic findings, and seven considered complications. CTC appeared cost-effective versus no screening and, in general, flexible sigmoidoscopy and FOBT, the authors found. However, results were mixed when comparing CTC with colonoscopy. The parameters that most influenced cost-effectiveness included CTC costs, screening uptake, threshold for polyp referral, and extracolonic findings.
"Given that FOBT is the most frequently used test in screening programs, future studies should focus on CTC versus FOBT (including newer versions of these tests) and the various alternative versions of FIT," Hanly and colleagues wrote.
Overdetection and overtreatment are usually concerns for cancer screening programs, but there is little evidence on these for colorectal cancer screening. For CTC, there are two areas where overdetection could be relevant: detecting polyps that may have never turned into cancer and detecting extracolonic lesions that may have never presented clinically.
Overdetection can be addressed in part by the appropriate choice of the polyp size threshold for referral to diagnostic intervention following CTC, according to the researchers. The Working Group on Virtual Colonoscopy recommends a 6- to 9-mm threshold for surveillance or referral to colonoscopy. Imposing referral standard threshold contradicts current gastroenterology practice of removing all polyps no matter the size, and the referral rate is still large and varies between studies.
"Future CTC studies -- on both effectiveness and cost-effectiveness -- should focus more explicitly on polyp overdetection," the authors stated.
CTC could play a huge role in extracolonic findings but uncertainty remains over whether detecting these findings is cost-generating or cost-saving, they added. Early detection may reduce future medical costs, but extensive follow-up after CTC may result in unnecessary investigations.
There are two key issues at play here: Extracolonic findings' prevalence among the general population is unclear, and estimation of associated costs has only been partially addressed. Studies so far have only addressed short-term costs, but long-term costs such as diagnostic workup, expert consultations, surgery, and treatment have not been considered.
In terms of screening uptake, the estimates appear "artificially high," outstripping real-world experience where uptake rarely exceeds 60% and usually falls below it. The assumption for increased screening uptake is predicated on CTC's lack of sedation and the less invasive nature of the test. However, because CTC is unable to take biopsies at the time of the test, patients seem to prefer colonoscopy, so the uptake level is probably lower than what is currently predicted. Improving accuracy of uptake estimates should be a key objective for future studies, according to Hanly and colleagues.
"More emphasis should be placed on exploring asymptomatic individuals' views, preferences, and experiences of fecal tests and FS compared with CTC," they noted.
Another reason Hanly and colleagues cannot come to any definitive conclusions about CTC is there isn't any evidence of CTC's ability to reduce mortality in the population. Current evidence mainly comes from cross-sectional studies on test performance characteristics. Cost-effectiveness studies that are more representative of an average screening population tended to result in CTC not being considered cost-effective compared with relevant alternatives. Also, the effectiveness measures tended to concentrate on sensitivity and specificity, neglecting measures of quality of life. More research is needed to better understand the quality-of-life impact across the entire screening process and future cost-effectiveness analyses should take these into account.
Also, many cost-effectiveness studies projected that CTC screening would reduce the number of colonoscopies required and transfer the burden from endoscopic services to radiologic services. However, all studies indicated CTC wouldn't replace colonoscopy or FOBT but would be employed in a complementary way.
Questions remain: Can CTC demonstrate high consistency and sensitivity across a range of settings, overcome issues with regard to optimal technological characteristics of the technique particularly in relation to referral size threshold, overcome procedure costs, and surmount risks from radiation exposure?
Future cost-effectiveness analyses should model clinically appropriate CTC screening scenarios with 10-yearly screening intervals and a polyp referral threshold of 6 mm or 10 mm, make more realistic assumptions regarding screening uptake, and include a range of costs, the authors concluded.
"They should focus on comparing CTC to fecal tests ... and FS, the tests more commonly used in screening programs," they added. "Comprehensive multivariate sensitivity analyses are required to fully understand how results depend on parameter estimates. Finally, the long-term costs and benefits emanating from detection of extracolonic findings require more serious consideration."