Univariate analysis shows many radiomic features have significant prognostic value in prostate cancer cases, but when included in multivariable models, these features do not improve predictive accuracy over clinical features alone, an Australian study has found.
"This suggests that radiomic features may not provide additional prognostic power for predicting overall survival in this cohort, and clinical features continue to be the most effective tool for prognosis," noted medical physicist Kaylee Molin and colleagues at the University of Western Australia (UWA), adding that the findings suggest the incorporation of radiomic features into routine clinical practice requires further investigation.
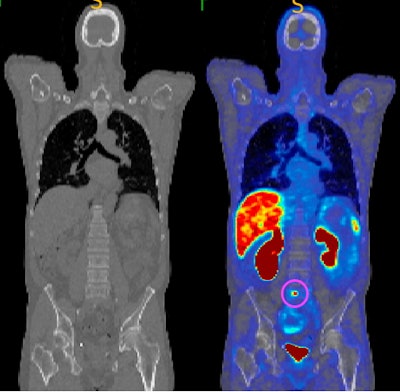 CT image (left) and gallium-68 (Ga-68) PSMA-11 PET/CT (right) showing an identified tumor circled in pink, which is not visible on the CT scan. This modality uses a radioactive tracer that targets tumors by binding to overexpressed PSMA in cancer cells. PSMA PET/CT offers high sensitivity and specificity, with studies showing it has higher detection rates compared to conventional imaging. All figures courtesy of Kaylee Molin, Martin Ebert et al and presented at the Royal Australian and New Zealand College of Radiologists (RANZCR) Annual Scientific Meeting (ASM).
CT image (left) and gallium-68 (Ga-68) PSMA-11 PET/CT (right) showing an identified tumor circled in pink, which is not visible on the CT scan. This modality uses a radioactive tracer that targets tumors by binding to overexpressed PSMA in cancer cells. PSMA PET/CT offers high sensitivity and specificity, with studies showing it has higher detection rates compared to conventional imaging. All figures courtesy of Kaylee Molin, Martin Ebert et al and presented at the Royal Australian and New Zealand College of Radiologists (RANZCR) Annual Scientific Meeting (ASM).
Prostate cancer is the second leading cause of cancer-related mortality among men, after lung cancer, and when it metastasizes, the five-year survival rate drops from nearly 100% to just 30%, the researchers explained. If the cancer returns after primary therapy, it is termed biochemically recurrent prostate cancer, marked by an increase in prostate-specific antigen (PSA) levels.
"Recent advancements in imaging technologies and the field of radiomics -- whereby a large number of quantitative features are extracted from medical images -- offer promising avenues for enhancing prognostic accuracy and for better patient risk stratification," the team wrote in an article posted on 9 January 2025 by Physical and Engineering Sciences in Medicine. "Radiomics can capture subtle tumor characteristics and biomarkers, providing valuable diagnostic or prognostic information, with the potential to aid clinical decision-making."
In research first presented at the 2024 RANZCR ASM, they sought to identify at-risk patients by developing predictive models for overall survival, using radiomic features from baseline gallium-68 (Ga-68) prostate-specific membrane antigen (PSMA)-11 PET/CT scans combined with clinical features.
Molin and colleagues conducted a multicenter study involving 180 patients with biochemically recurrent metastatic prostate cancer at Sir Charles Gairdner Hospital, Nedlands, and Fiona Stanley Hospital, Murdoch, both located in Western Australia.
All patients underwent Ga-68 PSMA-11 PET/CT imaging, and the analysis consisted of univariable and multivariable phases. The univariable analysis (shown in the figure below) correlated individual features with overall survival using Kaplan-Meier curves and Cox proportional hazards models. The multivariable analysis involved creating Cox proportional hazards models for predicting overall survival using clinical features only, radiomic features only, and various combinations of both, resulting in 13 models, the authors explained.
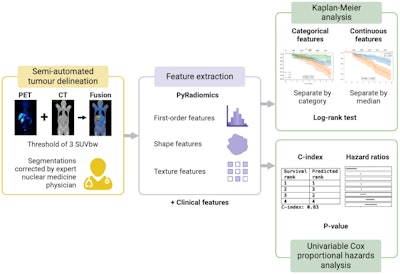 Workflow for univariable analysis. First, the regions of uptake greater than three standardized uptake values normalized by body weight were automatically segmented and corrected by an experienced nuclear medicine physician. Then, radiomic features were extracted from the largest/hottest/weighted average of the largest three lesion/s and combined with the patient's clinical features. Univariable analysis was performed using Kaplan-Meier curves and the log-rank test. Categorical features were separated by group, and continuous features were dichotomized based on the median value. A univariable Cox proportional hazards analysis was also conducted to determine the hazard ratios, concordance indices, and significant features, based on a p-value of less than 0.05.
Workflow for univariable analysis. First, the regions of uptake greater than three standardized uptake values normalized by body weight were automatically segmented and corrected by an experienced nuclear medicine physician. Then, radiomic features were extracted from the largest/hottest/weighted average of the largest three lesion/s and combined with the patient's clinical features. Univariable analysis was performed using Kaplan-Meier curves and the log-rank test. Categorical features were separated by group, and continuous features were dichotomized based on the median value. A univariable Cox proportional hazards analysis was also conducted to determine the hazard ratios, concordance indices, and significant features, based on a p-value of less than 0.05.
In the univariable analysis, 68 out of 89 radiomic features (76%) from the largest lesion were significantly correlated with overall survival (p-value < 0.05) using a univariable Cox proportional hazards model. The top radiomic features with the highest C-indices were: total lesional uptake, C-index = 0.707, p = 7.26×10-8; total lesional volume, C-index = 0.704, p = 2.16×10-7; original Gray Level Dependence Matrix (GLDM) dependence entropy, C-index = 0.704, p = 3.12×10-7.
In total, six out of eight clinical features were highly correlated with overall survival: prostatectomy vs radiotherapy, number of lesions, baseline PSA level, conventional staging, PET/CT-based staging, and age.
In the multivariable analysis, optimism-corrected 95% confidence intervals for the C-indices for the largest lesion: clinical-only model, 0.722 (95% CI: 0.653-0.784); radiomics-only model, 0.681 (95% CI: 0.616-0.745); and combination model (three radiomics + three clinical features), 0.704 (95% CI: 0.648-0.768).
Although radiomic features did not improve the multivariable survival models, the univariable analysis revealed significant correlations between many radiomic features and overall survival, according to the researchers.
"Ongoing studies are focusing on correlating RECIP 1.0 and PPP prostate cancer response evaluation criteria with patient overall survival and biochemical progression in our cohort," corresponding author Martin Ebert, PhD, director of physics research at WA Health and adjunct professor at UWA, told AuntMinnieEurope.com on 12 February.
The group also had a paper published in European Radiology on 10 January 2025 (Evaluating the impact of the Radiomics Quality Score: a systematic review and meta-analysis, https://doi.org/10.1007/s00330-024-11341-y).
To read the Physical and Engineering Sciences in Medicine paper, click here. Also, you can view the full e-poster on the EPOS section for the 2024 RANZCR ASM via the ESR's website. The co-authors were Nathaniel Barry, Suki Gill, Mubashar Hassan, Roslyn Francis, Jeremy S.L. Ong, Martin Ebert, and Jake Kendrick.