Radiology is uniquely positioned to have a pivotal role in shaping a more compassionate approach to mortality, according to two leading researchers in postmortem imaging.
By increasing awareness of radiology's contributions, systems and procedures can be developed that respect cultural sensitivities and support grieving families, according to Dr. Susan Shelmerdine, PhD, consultant academic pediatric radiologist at London's Great Ormond Street Hospital, and Dr. Natasha Davendralingam, consultant radiologist at the Tameside and Glossop NHS Foundation Trust, Ashton-under-Lyne, U.K.
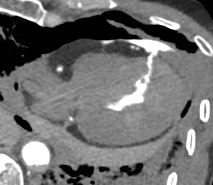
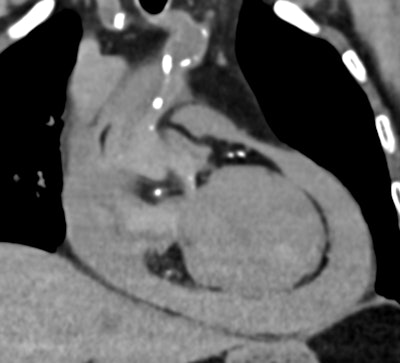 Postmortem CT reveals a large-volume hemopericardium caused by myocardial rupture, providing a definitive cause of death and avoiding the need for an invasive autopsy. All images courtesy of Drs. Susan Shelmerdine and Natasha Davendralingam.
Postmortem CT reveals a large-volume hemopericardium caused by myocardial rupture, providing a definitive cause of death and avoiding the need for an invasive autopsy. All images courtesy of Drs. Susan Shelmerdine and Natasha Davendralingam.
In a letter posted by the BMJ on 23 January, they responded to articles published in the journal's Christmas 2024 edition that called for death to be "demedicalized" and urged healthcare systems to focus on compassion and care for people who are dying. This conversation has centered on palliative care, but radiology often gets overlooked, they noted.
"Conventional autopsies are invasive and emotionally distressing for grieving families," wrote Shelmerdine, who is also an associate professor at the Great Ormond Street UCL Institute of Child Health, and Davendralingam. "Moreover, a shortage of pathologists has led to extended waiting periods before families receive answers. These delays prolong grief and hinder opportunities for emotional closure. By contrast, postmortem imaging offers a dignified alternative, providing timely and accurate information that also respects cultures or religions where invasive autopsies are taboo."
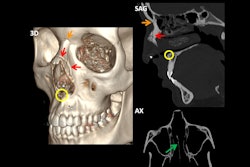
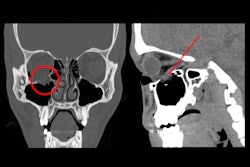
 Postmortem CT with coronary angiography and positive contrast highlights the precise location of myocardial rupture within the left ventricular wall, showcasing the value of contrast-enhanced imaging in providing accurate diagnoses without the need for autopsy.
Postmortem CT with coronary angiography and positive contrast highlights the precise location of myocardial rupture within the left ventricular wall, showcasing the value of contrast-enhanced imaging in providing accurate diagnoses without the need for autopsy.
Postmortem imaging with CT and MRI is also important for cases of stillbirths and miscarriages when it can offer insights into whether conditions are likely to recur in future pregnancies, guide genetic testing, or, when findings are normal, provide much-needed reassurance to parents that the loss was not their fault, they continued.
"Despite this promise, postmortem imaging remains an underused resource. Currently, it is not part of standard National Health Service (NHS) care and is often funded by local authorities or directly by bereaved families. Although some coroners have embraced this technology, others have not--leaving families to navigate a complex, slow, and often opaque system," wrote Shelmerdine, who is a member of the European Society of Paediatric Radiology postmortem imaging taskforce, and Davendralingam, who is a member of the International Society of Forensic Radiology and Imaging guidelines committee.
Tackling these challenges requires coordinated efforts to develop sustainable funding mechanisms and establish training pathways for radiologists to learn this important skill, they added.
 Drs. Susan Shelmerdine (right) and Natasha Davendralingam are co-founders of Anubix, a company that provides postmortem radiology reporting services.
Drs. Susan Shelmerdine (right) and Natasha Davendralingam are co-founders of Anubix, a company that provides postmortem radiology reporting services.
The two researchers have received an invitation from BJR Open to write an article on medicolegal considerations in postmortem imaging, and they intend to work on this in due course. To find out more, you can also check out these recent articles:
Davendralingam N, Brookes AL, Shah MA, Shelmerdine SC. Post-mortem CT service structures in non-suspicious death investigations. BJR Open 2024;6:tzae036. doi: 10.1093/bjro/tzae036. pmid: 39552614.
Shelmerdine SC, Arthurs OJ. How to report perinatal and paediatric postmortem CT. Insights Imaging. 2024 May 31;15(1):129. doi: 10.1186/s13244-024-01698-5. PMID: 38816589; PMCID: PMC11139809. https://pubmed.ncbi.nlm.nih.gov/38816589/
Shelmerdine SC, Davendralingam N, Langan D, Palm L, Mangham C, Arthurs OJ; CORNRD Study Collaborators. Post-mortem skeletal survey (PMSS) versus post-mortem computed tomography (PMCT) for the detection of corner metaphyseal lesions (CML) in children. Eur Radiol. 2024 Sep;34(9):5561-5569. doi: 10.1007/s00330-024-10679-7. Epub 2024 Mar 9. PMID: 38459348. https://pubmed.ncbi.nlm.nih.gov/38459348/