Radiologists must get up to speed on the diverse causes of stroke in younger people to ensure an accurate imaging workup. This facilitates early identification, determination of underlying etiology, and assessment of vascular involvement, all of which are critical for tailoring therapeutic strategies and improving long-term prognosis, prizewinning Spanish researchers have emphasized.
"The incidence of ischemic infarction is rising among adolescents and young adults, emerging as a public health concern, due to significant morbidity and extended disability in this age group," noted Dr. Ana Berasategui Criado, from Hospital Universitario Marqués de Valdecilla, Universidad de Cantabria, Santander, and colleagues. "Imaging is critical for characterizing stroke subtypes, identifying underlying causes, and assessing vascular abnormalities, guiding subsequent management."
Prompt and accurate diagnosis is paramount for a positive outcome, and a multidisciplinary approach involving radiologists and clinicians is imperative in managing juvenile stroke and ensuring timely intervention and optimal care, they explained in an e-poster presentation that received a Cum Laude award at ECR 2024.
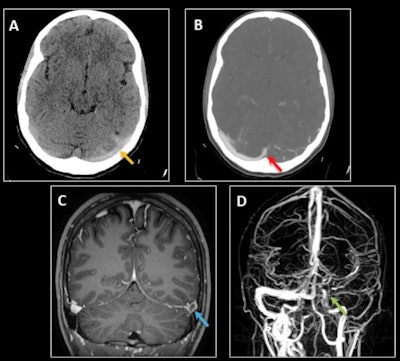 Cerebral venous thrombosis in a 25-year-old woman with a two-week history of left-sided oppressive hemicranial headache and neck pain. (A) Nonenhanced CT shows hyperattenuation of the left transverse and sigmoid sinuses (dense sinus sign) with cortical venous engorgement (yellow arrow). (B) Venous CT angiography shows a filling defect involving the left transverse sinus up to the confluence with the superior sagittal sinus (red arrow), the sigmoid sinus, and the intracranial internal jugular vein. (C-D) MRI sequences confirm a filling defect after gadolinium administration in the left transverse sinus (empty delta sign, blue arrow in C), and the absence of signal on the 3D time-of-flight venous sequence in the left sigmoid and transverse sinuses up to the torcula and in the middle and lower thirds of the superior sagittal sinus (green arrow in D). Factor V Leiden Mutation was disovered. (All images courtesy of Dr. Ana Berasategui Criado et al and presented at ECR 2024).
Cerebral venous thrombosis in a 25-year-old woman with a two-week history of left-sided oppressive hemicranial headache and neck pain. (A) Nonenhanced CT shows hyperattenuation of the left transverse and sigmoid sinuses (dense sinus sign) with cortical venous engorgement (yellow arrow). (B) Venous CT angiography shows a filling defect involving the left transverse sinus up to the confluence with the superior sagittal sinus (red arrow), the sigmoid sinus, and the intracranial internal jugular vein. (C-D) MRI sequences confirm a filling defect after gadolinium administration in the left transverse sinus (empty delta sign, blue arrow in C), and the absence of signal on the 3D time-of-flight venous sequence in the left sigmoid and transverse sinuses up to the torcula and in the middle and lower thirds of the superior sagittal sinus (green arrow in D). Factor V Leiden Mutation was disovered. (All images courtesy of Dr. Ana Berasategui Criado et al and presented at ECR 2024).
"Modifiable risk factors are responsible for nearly 80% of ischemic strokes in young individuals, with cardioembolic stroke being the most common," the authors pointed out. "Imaging algorithms must cover hemorrhage exclusion, assess stroke mimics, and consider eligibility for intra-arterial therapy."
CT is the gold standard in the acute setting enabling hemorrhagic stroke exclusion and early ischemic change detection, while MRI can provide higher sensitivity with faster acquisition times. MRI protocols with diffusion-weighted imaging (DWI), gradient-echo, FLAIR sequences, MR angiography, and post-contrast perfusion can also be useful, they added.
"CT/MR angiography provides rapid and precise vascular interpretation. Venous imaging must be included in young adults. Perfusion images are crucial in juvenile stroke, aiding in selecting candidates for endovascular treatment by assessing the infarct core," the researchers explained. "Vessel wall imaging (VWI) uses black blood sequences and pre/postcontrast acquisitions and differentiates intracranial diseases by evaluating stenosis, concentric/eccentric nature, location, and enhancement. Conventional catheter angiography remains the gold standard for intracranial steno-occlusive diseases, nonatherosclerotic vasculopathy, and planned revascularization."
In cases of cardioembolism, imaging can reveal multifocal infarcts in various arterial territories due to emboli release or solitary embolus causing a single vascular territory infarct. Bland emboli heighten the risk of ischemic stroke and silent cerebral infarction syndrome. Linked with cardiac masses, arrhythmias, dilated cardiomyopathy, and paradoxical thromboembolism, they typically manifest as multifocal small infarcts in various arterial territories, they added.
Cerebral embolization caused by atrial myxoma leads to infarction, aneurysm, and metastasis. Aneurysms, often multiple and hyperdense on noncontrast CT (mixoid matrix, wall calcification), favor middle cerebral artery distal branches. Metastases appear as multiple, typically frontoparietal hemorrhagic masses, according to the Santander team. Septic emboli, linked to endocarditis, most commonly course with small scattered ischemic infarcts. Other findings include abscesses, intraparenchymal/subarachnoid hemorrhage, and mycotic aneurysms.
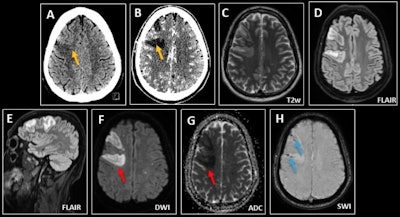 Septic emboli in a 40-year-old man with headache and acute confusional state in the context of bacterial endocarditis. (A-B) CT demonstrates a focal area of right frontal cortical edema, more evident in the postcontrast phase (yellow arrows), compatible with a subacute infarct or low-grade neoplasia. (C-G) MRI shows multiple scattered foci of increased intensity on T2/FLAIR, with restricted diffusion in both cerebral hemispheres, suggesting embolic infarcts (red arrows). (H) Dominant right frontal lesions associate microhemorrhage on susceptibility-weighted imaging (blue arrows).
Septic emboli in a 40-year-old man with headache and acute confusional state in the context of bacterial endocarditis. (A-B) CT demonstrates a focal area of right frontal cortical edema, more evident in the postcontrast phase (yellow arrows), compatible with a subacute infarct or low-grade neoplasia. (C-G) MRI shows multiple scattered foci of increased intensity on T2/FLAIR, with restricted diffusion in both cerebral hemispheres, suggesting embolic infarcts (red arrows). (H) Dominant right frontal lesions associate microhemorrhage on susceptibility-weighted imaging (blue arrows).
"Cerebral fat embolism syndrome tends to develop in patients with large displaced fractures or sickle cell anemia," they noted. "In the acute phase, MRI shows a 'starfield' pattern with multiple scattered foci of diffusion restriction and FLAIR hyperintensity in the white matter, corpus callosum, basal ganglia, thalamus, brainstem, and cerebellum."
In the subacute phase, confluent areas of diffusion restriction appear in subcortical and deep white matter, and microhemorrhages in areas of cytotoxic edema may appear. Air emboli result from invasive procedures causing contact between the external environment and the vascular system under an atmospheric pressure gradient. Proximal introduction before aortic branching leads to scattered infarcts across multiple vascular territories. Air introduction in carotid/vertebrobasilar procedures restricts infarcts to a specific vascular territory, they wrote.
Atherosclerosis, uncommon in young individuals, is linked to cardiovascular risk factors, causing thromboembolic, hypoperfusion, or mixed strokes. CT/MR angiography reveals calcified/noncalcified atherosclerotic plaques with stenosis, while VWI highlights eccentric wall enhancement. Plaque features like ulceration, fibrous cap thickness, and necrotic core predict stroke, according to the authors.
Cervical arterial dissection, a major cause of juvenile stroke, may be spontaneous or traumatic, involving thromboembolic stroke (80%), hypoperfusion, and mixed mechanisms. Up to 10% experience bilateral dissection. CT/MR angiography reveals irregular filiform stenosis (string of pearls sign), narrowing to a point (flame sign), mural thickening (crescent sign), or an intimal flap, they wrote.
Drug abuse is a major cause of ischemic stroke in young adults, concerning hypertension, arrhythmias, vasospasm, vasculitis, thrombosis, cardioembolism, and injected material embolization, leading to encephalopathy, hemorrhage, or ischemic infarction, they pointed out.
The co-authors of the ECR 2024 poster were Marina Arroyo Olmedo, Celia Cantolla, Sofia Maria Bretos Azcona, Alejandra Somoano, Silvia Revuelta Gómez, Rodrigo Sutil, Aranzazu Sánchez Gabín, and David Castanedo Vázquez.