Marking 50 years of CT (1971 to 2021), the UK Imaging & Oncology Congress (UKIO 2021, 7 to 25 June) kicked off on Monday with an online plenary session, "CT at 50," in honor of the modality's golden jubilee.
Prof. Dame Janet Husband, whose own four-decade career in CT and cancer imaging is nearly as long-standing, presented the keynote talk, which was followed by a question-and-answer session in which she addressed trends and challenges in the modality.
Husband is founder and president of the International Cancer Imaging Society, and she describes her role in the development of CT as a cancer imaging tool as "lucky," dictated more by the need to train and work part time due to family commitments than by an overriding passion for radiology. Then a life-changing moment made her realize CT's breathtaking potential and she never looked back.
 Prof. Dame Janet Husband pictured here with Imogen, the mascot of the International Cancer Imaging Society (ICIS). Photo courtesy of ICIS.
Prof. Dame Janet Husband pictured here with Imogen, the mascot of the International Cancer Imaging Society (ICIS). Photo courtesy of ICIS.When Husband first started training in radiology, it was a specialty that took place "behind closed doors" and was based predominantly on still or cinematic x-ray. Radiologists seemed to have no interaction with patients. The turning point came in April 1972, when she attended a lecture given by Dr. James Ambrose and Sir Godfrey Hounsfield on the first clinical results for CT.
"We were late for the session and had to stand at the back of the room, and at the end of the lecture you could have heard a pin drop. The whole audience was absolutely amazed," Husband noted. "We could hardly take in what we'd seen. It was one of the great highlights of my life to be there at that time."
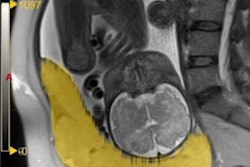
She noted how the images in Ambrose's talk revealed a tumor for the first time, rather than it merely being inferred through a barium meal.
Husband trained four mornings a week but missed the encephalography training, as all the neuro examinations took place in the afternoon. She described herself back then as a "half-baked radiologist" when she received her Fellow of the Royal College of Radiologists certification.
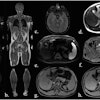
However, this was to change when she joined Northwick Park Hospital, where she worked with Dr. Louis Kreel as a part-time research fellow from May 1976 on the prototype of the first body CT scanner, which had been installed in late 1975.
"As soon as the body scanner was introduced, it was like switching on a light in a dark room. Suddenly you could see inside the body. It was amazing," noted Husband. "It became clear very quickly that CT was going to be a really important tool in diagnosing and assessing patients with cancer."
Cost hurdles
But was it affordability or resistance that put the brakes on CT adoption? Responding to this question put to her by attendee Dr. Adrian Thomas during the Q&A, Husband noted there was a need to understand the value of CT for patient management. Some education was required, but Husband remembers both clinicians and radiologists being excited by CT's potential.
The real issue was CT's prohibitive cost. While there are doubts about the veracity of the rumor that EMI funded the research with money from its sales of Beatles' music, what is certain is that once the technique was established, it would be decades before the government bought scanners. Most of the first ones in clinical practice during the 1980s were funded by charities.
Chair of the plenary session Dr. Nick Spencer asked Husband which she considered to be the greatest revolution, CT or MRI. In terms of its impact when it was first introduced, Husband is clear: CT. She described its adoption in clinical practice as mind-blowing, noting that it is now ubiquitous due to its speed and spatial coverage.
Spencer also quizzed her on which factor was more important for CT development, helical hardware or computing power. Again, there was no hesitation: computing power, as whole-body scans can now be undertaken and processed in a very short amount of time, she noted.
Bright future
And what is on the horizon for CT, in 50 years' time when CT is celebrating its 100th anniversary? While for the moment CT technology seems to have plateaued, Husband pointed to artificial intelligence (AI) as the next big thing to be incorporated into the modality, and this will further impact exam time. Responding to one listener, she noted that AI and radiomics via computing power were likely to be the next greatest advances.
AI won't replace radiologists, but it will be valuable for first reads and selecting individual cases that need to be read before the others, according to Husband, but it won't help with the longer-term shortage of radiologists and radiographers. In response to another question, Spencer also pointed to AI's potential in the diagnosis of dementia due to its capacity to make comparative measurements of brain atrophy patterns.
One listener asked whether CT should be limited in follow-up or used as needed? When it comes to new drugs for treatment, imaging is needed at certain time points in any therapy trial, she noted.
However, for the long-term follow-up of individuals, it may be possible to reduce scans and lengthen intervals, she said, adding that this constituted a difficult challenge as no two patients are the same. She also flagged how COVID-19 had introduced the virtual consultation and this trend was likely to continue in medicine, impacting hospital attendance and the number of scans undertaken.
Now she can't think of a more exciting field of medicine to work in than imaging. For any young medics considering imaging, she had the following advice:
"Keep going, it's a fascinating specialty, and there will be something for everyone -- whether it's interventional, cardiac, or breast imaging -- you can become an expert in a small area."
She also underlined that a multidisciplinary approach was crucial not just in CT but in cancer management.
"Together we can solve the list of problems as we go through into the next era of computer medicine," she said.