What do the specialists say when it comes to the notoriously tricky area of CT evaluation of lung parenchyma? ECR 2021 registrants received sound, practical advice from expert speakers at a special focus session.
Cystic abnormalities are often challenging to interpret, given the significant crossover in their imaging appearance; a variety of entities result in these abnormalities and radiologists need to approach them carefully on CT, according to Prof. Peter Beddy, consultant radiologist at St. James' and Beacon Hospitals in Dublin and senior lecturer at Trinity College Dublin.
The true lung cyst is a well-defined, rounded lesion with a thin wall, usually containing air, and it can be an isolated abnormality or part of a cystic lung disease, noted Beddy, whose presentation focused on differentiating cystic lesions from emphysema.
"Conventional wisdom in thoracic imaging was that patients do not develop simple lung cysts as they do in the liver and kidney," he said. "With increasing availability of CT, we are beginning to recognize that patients can develop lung cysts as they get older. This may be the result of previous infection or trauma; however, the frequency of incidence suggests that it may occur spontaneously."
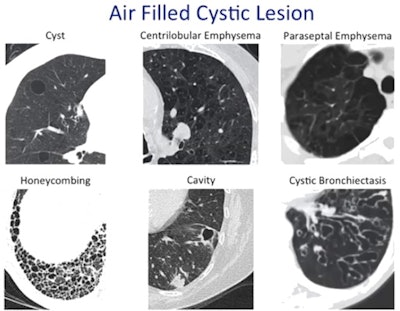 Various entities cause air-filled cystic lesions which need differentiation on CT. Courtesy of Prof. Peter Beddy.
Various entities cause air-filled cystic lesions which need differentiation on CT. Courtesy of Prof. Peter Beddy.He cautioned against dismissing isolated cysts as benign entities entirely because radiologists increasingly are recognizing a cystic tumor that develops from what has been described previously as a simple cyst. Multiple cysts, on the other hand, must trigger suspicion of cystic lung disease such as Langerhans cell histiocytosis or lymphangioleiomyomatosis. One of its main differentials, however, is emphysema.
Wall scrutiny
It can be difficult to differentiate centrilobular emphysema from cystic lung disease, but attentive assessment will help in most cases.
Two key features are crucial to differentiation, Beddy explained. The first is the wall, which is not present in most emphysema, unless it is advanced and the result of fibrosis. In emphysema, however, this type of wall is usually incomplete and therefore can be differentiated from a lung cyst. The second is the presence of internal architecture which in centrilobular emphysema may present as a central dot, representing a vessel within the area of destroyed lung.
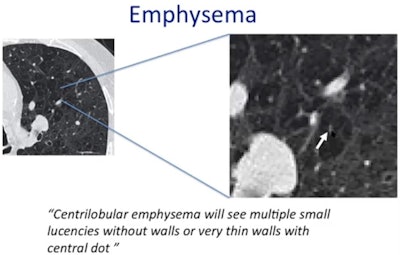 Centrilobular emphysema has no or very thin walls and a central dot. Courtesy of Prof. Peter Beddy.
Centrilobular emphysema has no or very thin walls and a central dot. Courtesy of Prof. Peter Beddy."The key difference between centrilobular emphysema and a lung cyst is that emphysema lacks a perceptible wall in most cases, and will have an internal structure, whereas a cyst has a definable wall and no internal structure," he said.
Radiologists should therefore ask themselves: Does the lesion have internal contents? Does it have a wall? The essential point is to check this wall not just for differentiating centrilobular emphysema but also for ruling out other differentials.
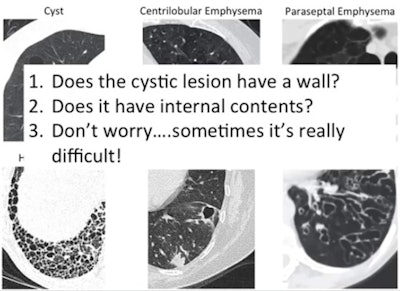 Three top tips for determining pathology in air-filled cystic lesion. Courtesy of Prof. Peter Beddy.
Three top tips for determining pathology in air-filled cystic lesion. Courtesy of Prof. Peter Beddy.For example, lung cavities have thick irregular walls, whereas the subpleural lucencies of paraseptal emphysema often share very thin walls. Meanwhile, honeycombing presents as air-filled cystic spaces in peripheral and subpleural locations with well-defined walls, he noted.
Honeycombing and paraseptal emphysema
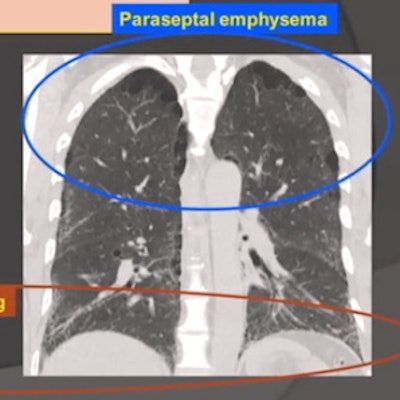
During the same ECR session, Prof. Johny Verschakelen, professor of radiology at the Catholic University of Leuven in Belgium, outlined the numerous challenges of differentiating between honeycombing and paraseptal emphysema.
"Always be aware of the fact that if you make a diagnosis of honeycombing, you have to be sure because you are indicating that this patient has irreversible fibrosis," he said.
On CT, both entities appear as millimetric to centimetric lucent spaces, but while honeycombing is surrounded by irregular coarse lines, paraseptal emphysema is surrounded by smooth, fine lines.
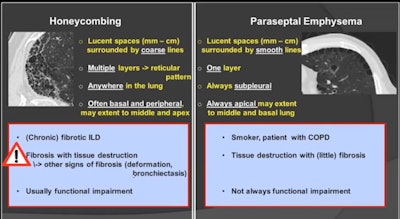 CT signs of honeycombing versus paraseptal emphysema. Courtesy of Prof. Johny Verschakelen.
CT signs of honeycombing versus paraseptal emphysema. Courtesy of Prof. Johny Verschakelen.Furthermore, in honeycombing, multiple layers of these lucent spaces look like a reticular pattern, and they can be anywhere in the lung. In paraseptal emphysema, only one layer of lucent spaces can be seen, and these are always subpleural. This includes the subpleural fissure area, according to Verschakelen.
Honeycombing is often basal and peripheral but may extend to the middle and apex of the lung, and with this distribution, it is highly suggestive of usual interstitial pneumonia (UIP) in the setting of idiopathic pulmonary fibrosis (IPF). On the other hand, paraseptal emphysema is always apical and may extend to the middle and basal lung.
Patient history
It is crucial to look at the clinical context, he continued. The presence of sometimes extensive honeycombing may indicate that the patient has chronic fibrotic interstitial lung disease.
"Honeycombing is a fibrotic process -- the result of extensive fibrosis with tissue destruction. This means that usually in addition to the honeycombing, you'll see some other small signs of fibrosis like lung deformation or traction bronchiectasis. The fibrosis usually induces functional impairment," Verschakelen said.
A patient with paraseptal emphysema could be a smoker or have chronic obstructive pulmonary disease, he added. Here, the process starts with tissue destruction and little fibrosis, and these patients don't always have functional impairment. Paraseptal emphysema may even be an incidental finding.
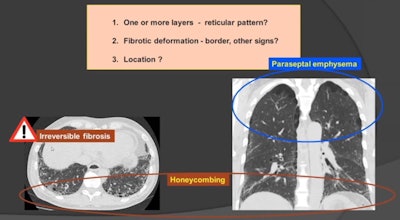 Location is the key when it comes to differentiating honeycombing from paraseptal emphysema. Courtesy of Prof. Johny Verschakelen.
Location is the key when it comes to differentiating honeycombing from paraseptal emphysema. Courtesy of Prof. Johny Verschakelen.Verschakelen's top tip for differentiation of honeycombing and paraseptal emphysema is that radiologists should ask themselves two questions: Is there more than one layer and/or a reticular pattern? Is there fibrotic deformation with irregular borders or other signs of deformation? For both questions, a positive answer means that honeycombing is the most likely diagnosis. However, location is key. If hyperlucent spaces are limited to the upper part of the lung in the subpleural area, then paraseptal emphysema is more likely.