German and Swiss researchers have developed a PET-based risk classification metric for prostate cancer patients to help predict their survival without disease recurrence. They published their findings on 16 March in the European Journal of Nuclear Medicine and Molecular Imaging.
The approach establishes prostate-specific antigen (PSA) parameters from prostate-specific membrane antigen (PSMA)-PET imaging to calculate patients' chances for relapse-free outcomes after radiotherapy and/or metastasis-directed therapy. As one might expect, the greater the PSA level, the greater the risk for disease recurrence. At the same time, patients with bone metastases were at higher risk of prostate cancer relapse, regardless of PSA levels, but still showed "satisfactory" recurrence-free survival.
"We developed a prognostic risk classification for biochemical relapse after PSMA-PET-guided [metastasis-directed therapy (MDT)] after [radical prostatectomy] with convincing internal validation," wrote the authors, led by Dr. Marco Vogel, from the department of radiation oncology at the Technical University of Munich. "This classification might be used to weigh the risk-benefit ratio of local curative [radiotherapy] for oligorecurrent lesions."
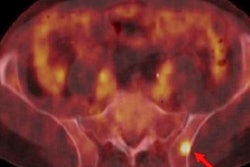
PSMA-PET utilization
The use of PSMA-PET to stage and target recurrent prostate cancer after radical prostatectomy has increased in recent years, as the modality provides radiation oncologists with better views of new tumors and distant lesions. With this additional insight, physicians can direct patients to more appropriate treatment, such as metastasis-directed therapy with conventional fractionated radiotherapy, stereotactic body radiotherapy, or surgery to extend survival and quality of life.
"Up to now, the optimal selection of patients for MDT is unknown. The majority of patients will develop progression, despite PSMA-PET staging and MDT," Vogel and colleagues wrote. "Therefore, clinical risk classifications have become an accepted instrument for weighing the risk-benefit ratio. To our knowledge, no such tools have been published for patients with oligorecurrent [prostate cancer (PC)] treated with MDT using highly sensitive PSMA-targeted imaging."
To fill that void, the researchers conducted a retrospective study and analyzed data from 292 patients (median age, 70 years; range, 46-95 years) who were treated for prostate cancer at one of six German and Swiss medical centers. The patients underwent conventional fractionated radiotherapy and/or stereotactic body radiotherapy between April 2013 and January 2018, as well as metastasis-directed therapy -- independent of the primary therapy -- for prostate cancer-related metastases.
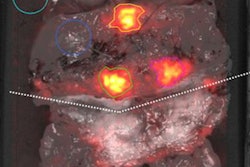
The cohort included patients with as many as five distant lymph node, bone, or visceral lesions and any level of PSA as determined by PSMA-PET diagnosis. There was no restriction on the total number of pelvic lymph node lesions.
Research criteria
Each patient underwent PET imaging approximately 60 minutes after injection with a gallium-68-labeled PSMA targeting ligand (mean activity, 162.5 MBq; range, 87-291 MBq), along with either low-dose, diagnostic CT or contrast-enhanced MRI. The primary end point was biochemical relapse-free survival, which was calculated from the time of metastasis-directed therapy to biochemical relapse (PSA level ≥ 0.2 ng/mL above the lowest point of PSA after radiotherapy). Median follow-up for the study's patients was 16 months (range, 0-57 months).
Variables in the analysis included initial tumor stage, initial nodal status, initial Gleason score, and initial resection status, along with risk factors based on PSA levels, PSA levels at PSMA-PET imaging and recurrence, the presence of pelvic lymph node lesions and distant metastases, and the number of lesions at the time of PSMA-PET.
While data on the prognostic value of PSA levels before metastasis-directed therapy in prostate cancer patients are rare, Vogel and colleagues' receiver operating characteristic (ROC) analysis determined that 0.8 ng/mL was the significant cutoff value for PSA before radiotherapy. "Although this value seems high, treatment of oligorecurrent PC appears to be beneficial when administered in patients with PSA levels < 0.8 ng/mL or preferably earlier," they wrote.
They then divided the subjects into four risk classes to calculate relapse-free survival based on the following criteria:
- Class I: PSA < 0.8 ng/mL, no bone lesions
- Class II: PSA ≥ 0.8 ng/mL, no bone or visceral lesions
- Class III: PSA < 0.8 ng/mL, bone lesions present
- Class IV: PSA ≥ 0.8 ng/mL, no bone lesions; visceral lesions present
Key PSA level
The analyses revealed that patients with a PSA level less than 0.8 ng/mL and local disease recurrence only had the longest mean duration for relapse-free survival.
| Mean relapse-free survival based on risk classification | ||||
| Class I, low risk | Class II, intermediate risk | Class III, high risk | Class IV, very high risk | |
| Mean relapse-free survival | 36.3 months | 25.8 months | 15.6 months | 5.7 months |
In addition, patients with bone metastases had a greater risk of their prostate cancer returning, regardless of PSA level, but still had a "satisfactory" chance for a relapse-free survival. Unfortunately, for patients with visceral metastases, their chances to remain free of disease and for extended survival were greatly decreased.
Based on the three most significant risk factors -- PSA level of at least 0.8 ng/mL and the presence of bone metastases and visceral lesions -- the researchers' risk classification achieved 70% accuracy.
This risk classification method might be used to weigh the risk-benefit ratio of local curative radiotherapy for prostate cancer lesions, Vogel and colleagues concluded; however, because patients with visceral metastases have a decreased chance of relapse-free survival, the use of metastasis-directed therapy should be evaluated on a case-by-cases basis, they concluded.