Researchers from Switzerland, Germany, and the U.S. have outlined the key applications of augmented reality (AR) in orthopedics and the technology's potential to save time, reduce risk, and enhance accuracy for image-guided procedures.
The group, led by Dr. Lukas Jud from the University of Zurich, performed a systematic search of major publication databases for studies using AR to facilitate orthopedic surgery. The researchers identified 31 studies on the topic, from which they drew information to outline the current state of understanding and research into relevant AR applications.
The integration of AR into medicine has grown considerably in recent years, particularly for image-guided neurointerventional procedures, the authors noted. There is also growing interest in applying AR to orthopedic surgery -- a specialty that relies heavily on medical images to plan and direct surgical procedures.
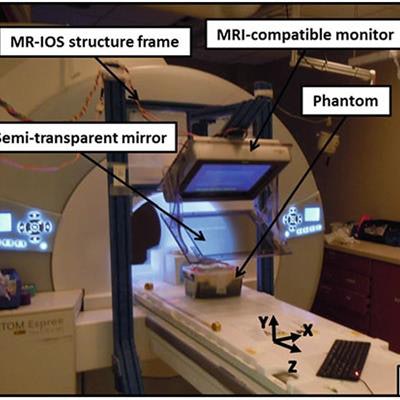
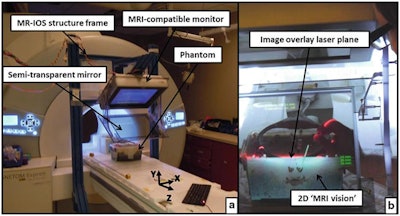 An augmented reality technique for MRI-guided musculoskeletal interventions. The Magnetic Resonance Image Overlay System (MR-IOS) allows users wearing an augmented reality headset to view a projection of MR images overlaid onto a patient lying on an MRI scanner bed. Image licensed under CC BY-NC 4.0.
An augmented reality technique for MRI-guided musculoskeletal interventions. The Magnetic Resonance Image Overlay System (MR-IOS) allows users wearing an augmented reality headset to view a projection of MR images overlaid onto a patient lying on an MRI scanner bed. Image licensed under CC BY-NC 4.0."To date, AR is not yet widely adopted in the clinical routine of orthopedic interventions. ... Nevertheless AR solutions seem to be well-suited for different interventions and are applicable to different fields of orthopedic surgery," they wrote (BMC Musculoskelet Disord, 15 February 2020, Vol. 21:103).
After examining the publications on using AR for orthopedics, the group divided the various AR applications mentioned into the following categories:
- Instrument and implant placement. In several studies, researchers used AR technology to create projections of patient anatomy based on CT and MRI data that they overlaid directly onto the patient to assist instrument and implant placement procedures.
For example, Wu et al used an AR-based camera setup to project spinal anatomy onto a patient to help clinicians identify optimal entry points for vertebroplasty. For a separate case study, U-Thainual et al developed an AR-based technique to allow for the visualization of MR images onto a phantom while simulating an MRI-guided musculoskeletal intervention.
AR technology can help reduce surgeons' need to map in their mind 2D images to the 3D anatomy of patients while planning and performing procedures, the authors noted. - Osteotomies. Surgeries involving the cutting of bones conventionally require a large number of x-ray images to complete. Intraoperative use of AR for osteotomies has the potential to reduce the amount of time patients spend under fluoroscopy and thus reduce their radiation exposure, as demonstrated by Fallavollita et al in a study of 25 human cadavers.
- Tumor surgery. AR also helped surgeons track the expansion of tumors in 3D, which contributed to an increase in accuracy for bone tumor resection, compared with the conventional technique, in multiple studies by Cho et al.
- Trauma. The planning of complex procedures to treat traumatic injuries can benefit from AR technology as well. Shen et al showed that the enhanced visualization of AR models of a fractured pelvis allowed clinicians to create an individually tailored implant for a patient. Intraoperative AR navigation also led to reductions in operation time for guide-wire insertion in several studies.
- Surgical training and education. AR has helped orthopedic surgeons and trainees simulate image-guided procedures. Several groups presented different AR-based training methods through which surgeons could advise and give feedback to trainees from a remote location. In addition, Condino et al introduced a patient-specific hybrid simulator that uses a combination of AR and 3D-printed models for orthopedic open surgery.
"Overall, AR has the potential to be a timesaving, risk and radiation reducing, and accuracy enhancing technology in orthopedic surgery ... [and] it can be expected that AR experiences a geometric increase in applicability in the field," the authors concluded.



















