What are the distinct benefits of 3D printing and augmented reality (AR) in the management of cardiac conditions, and what clinical scenarios are the technologies best suited for? Radiologists from Poland and Canada discussed these questions and more in a Thursday educational session at RSNA 2019.
"Though there are no specific clinical guidelines concerning when to use 3D printing over augmented reality for different clinical scenarios right now, we can say that AR and 3D printing complement each other and synergize well," presenter Dr. Jan Witowski told session attendees.
Numerous case studies have shown that patient-specific 3D-printed cardiac models have the potential to improve preprocedural planning and facilitate surgical simulation for various heart diseases, he added. AR may offer a cheaper alternative with a faster turnaround time that could be helpful for intraoperative guidance.
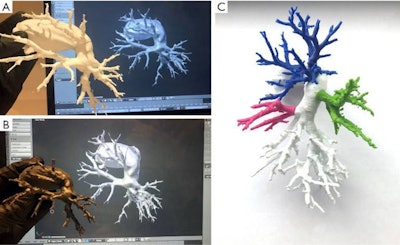 Patient-specific 3D-printed models of the pulmonary arteries and surrounding structures fabricated with white polylactic acid (A), flexible resin (B), and multipart polylactic acid (C). All images courtesy of Dr. Jan Witowski.
Patient-specific 3D-printed models of the pulmonary arteries and surrounding structures fabricated with white polylactic acid (A), flexible resin (B), and multipart polylactic acid (C). All images courtesy of Dr. Jan Witowski.Promising technologies
Early clinical results from the integration of AR and 3D printing in cardiac care have proven very promising, and cardiologists and cardiac surgeons have been seeking out ways to implement the emerging technologies in their daily work, Witowski noted. Witowski is affiliated with Jagiellonian University and will serve as a visiting fellow at Massachusetts General Hospital in early December.
Surgeons often ask radiologists to provide 3D visualization in addition to standard medical imaging before performing procedures. Though standard volume rendering is sufficient in many scenarios, AR and 3D printing can provide even more detailed information in an intuitive manner, which is especially critical for complex cases.
However, AR and 3D printing "need to be used in very specific scenarios," Witoswki said. "Not everyone will benefit from them, and it is important to know when and where we can think about them."
In the case of interventional cardiology procedures, clinicians at Witowski's institution have found the advanced visualization technologies to be useful for a variety of valvular and nonvalvular structural heart disease procedures as well as for vascular interventions. For example, they have used 3D-printed aortic roots to plan for and simulate transcatheter aortic valve replacement and AR models to guide endovascular aneurysm repair.
One recent case study on left atrial appendage closure showed that using a patient-specific 3D-printed model instead of 2D transesophageal echocardiography improved the accuracy of predicting the optimal occluder size (p = 0.03) and reduced total procedure time (p = 0.03). A separate group of researchers also from Poland demonstrated the viability of applying AR models to help guide the same procedure.
Though the workflow for creating AR and 3D-printed models is similar -- both entail image acquisition and segmentation followed by virtual 3D model generation -- AR production is much faster and cheaper because it does not require 3D printing of a physical model, Witowski noted. What's more, surgeons can examine AR models as digital overlays onto the patient or onto a real-time video feed while performing a procedure, which is not currently possible with 3D-printed models.
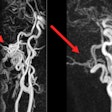
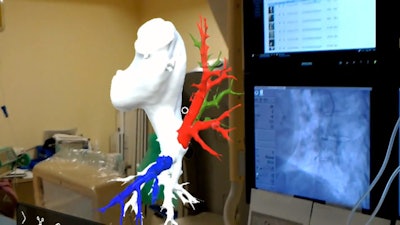 Augmented reality model of the pulmonary arteries and surrounding structures used to facilitate a percutaneous coronary intervention.
Augmented reality model of the pulmonary arteries and surrounding structures used to facilitate a percutaneous coronary intervention.Still, there is a much larger body of evidence supporting the potential benefits of patient-specific 3D-printed cardiac models for preprocedural planning and surgical simulation for various heart diseases, compared with AR models.
"3D printing, in general, is more realistic [than AR] right now because it has tissue and mechanical properties that allow it to be used for simulations," Witowski said. "However, AR is cheaper and faster, so if you want to perform an urgent case, or if you don't have enough resources to buy a high-end 3D printer, AR might be a good idea to consider."
As AR transitions out of its early phase, clinicians may start to use the technology more frequently for intraoperative situations and reserve 3D printing for surgical simulations and education, he said.
A 'must-have' tool
For congenital heart disease, 3D printing is no longer just a neat tool to use every once in a while. It has now become an essential part of preparing for surgical procedures, Dr. Shi-Joon Yoo, PhD, from the Hospital for Sick Children in Toronto, said.
Yoon and colleagues regularly create individually tailored 3D-printed models of pediatric patients based on free-breathing, whole-heart MR images acquired using a 1.5-tesla scanner at their institution.
They used several such 3D-printed models for an internal study involving 32 cases of congenital heart disease at the hospital. They found that simulating surgery on the models resulted in statistically significant improvements in various measures of surgical performance, such as fluency, knowledge, and respect for tissue, as well as reductions in average operating time (from approximately 1 hour and 26 minutes to 59 minutes).
"Simulation training of congenital heart surgery using 3D-printed models is now proven feasible, applicable, and, I would say, very, very powerful," he said. "Hands-on surgical training [with 3D-printed models] is not just an option anymore, it is a must-have."