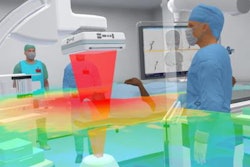
Virtual reality (VR) and 3D-printed models have demonstrated a potential to improve physicians' ability to classify acetabular fractures for surgery. Dutch researchers explored which of the two techniques was more effective to that end in a new study, published online in the European Journal of Orthopaedic Surgery & Traumatology.
The group, led by Dr. Lars Brouwers, created VR and 3D-printed acetabular models to determine which one of the two advanced visualization techniques best helped surgeons to correctly classify acetabular fractures and then choose the most appropriate surgical approach.
 A 3D-printed head model of a man who had a fork (red) lodged in his nose. The surgical team examined the 3D-printed model to plan the fork removal. All images courtesy of Dr. Lars Brouwers.
A 3D-printed head model of a man who had a fork (red) lodged in his nose. The surgical team examined the 3D-printed model to plan the fork removal. All images courtesy of Dr. Lars Brouwers."The study findings suggest that medical students can classify an acetabular fracture as well as the head of the trauma department of an academic hospital using 3D-printed models or virtual reality. The learning curve to identify fracture patterns is shortened ... and students can step in at a higher level than they did 20 years ago," first author Dr. Lars Brouwers told AuntMinnieEurope.com. Brouwers is a surgical resident and co-founder of the medical 3D lab at Elisabeth-Tweesteden Hospital in Tilburg (Eur J Orthop Surg Traumatol, 17 September 2019).
Classifying in 3D
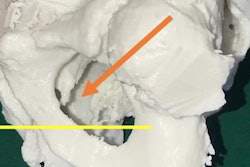
Accurately classifying hip joint fractures and preparing appropriate surgical treatment depends largely on patterns of injury visible on conventional CT scans. Unlike many other orthopedic injuries, however, acetabular fractures are especially challenging to diagnose and repair due to the complexity of the fracture lines and their susceptibility to improper wound closure.
Recently, emerging technologies such as VR and 3D printing have shown potential to improve fracture understanding and, as a result, allow clinicians to offer the best form of management.
"We think 3D printing is the next invention, after x-ray and CT, to improve fracture classification and preoperative planning," Brouwers said. "Using 3D-printed models, surgeons are able to expand their surgical preparations with a 3D view, whereas using conventional diagnostics require surgeons to form virtual 3D models in their heads."
In a prior study, Brouwers and colleagues examined the potential of 3D hip joint models, generated using VR and 3D printing technology, to facilitate physicians as they classified acetabular fractures and prepared for surgery. Their assessment indicated that using VR and 3D-printed models significantly increased interobserver agreement among physicians on fracture type and surgical approach, compared with conventional x-ray and CT scans.
Expanding upon this earlier work in their current study, the researchers set out to investigate whether 3D printing or VR was better for managing acetabular fractures. To that end, they asked physicians from various hospitals to classify 20 different acetabular fractures and determine the best surgical approach using either a 3D-printed model or 3D VR model.
 A 3D-printed vasculature model of a patient with an abdominal aneurysm who underwent endovascular aneurysm repair for a closed right iliac artery.
A 3D-printed vasculature model of a patient with an abdominal aneurysm who underwent endovascular aneurysm repair for a closed right iliac artery.They created the 3D-printed models by generating 3D reconstructions of pelvic CT scans using open-source software (Meshlab, Simplify 3D) and then printing them out using a 3D printer (Replicator Z18, Makerbot). They also used game development software (Unity, Unity Technologies) to create virtual environments suitable for visualizing the 3D reconstructions with a mobile VR headset (Gear VR, Samsung).
The study cohort consisted of 27 surgeons with varying degrees of experience managing acetabular fractures, from surgical interns to senior trauma surgeons.
Potential clinical value
Overall, Brouwers and colleagues found there was no statistically significant difference in the average amount of time it took the participants to classify acetabular fractures using a 3D-printed model (9.3 minutes) or a 3D VR model (10.7 minutes). There was also comparable interobserver agreement among the physicians in each group on choosing the ideal surgical approach and patient positioning, regardless of whether they examined a 3D-printed model or a 3D VR model.
However, the researchers did discover that using the 3D-printed models was associated with significantly greater interobserver agreement (Cohen's kappa coefficient of 0.47) among the physicians for classifying acetabular fractures, compared with the 3D VR models (kappa coefficient of 0.38). In contrast, the potential learning curve for treating acetabular fractures showed more improvement with VR than with 3D printing.
Following the tests, the participants commented on the advantages and disadvantages of using the two techniques. Regarding fracture classification, they commented that the 3D-printed model offered a more natural view but had some small details fused together, whereas the 3D VR models also provided a good 3D view with insight into fracture patterns but with limited rotation capabilities. For preoperative planning, the physicians claimed that the tangible nature of the 3D-printed models made them easier to use, although VR revealed more fine details.
The collective results suggest VR is slightly inferior to 3D printing in helping surgeons visualize and treat acetabular fractures. Nonetheless, any process that facilitates the classification of such a complex injury may be beneficial to patient care, the authors noted.
"The 3D printing industry sometimes sees 3D printing as the Holy Grail," Brouwers said. "However, we have to be critical. If you treated one case with a 3D-printed model and you are satisfied with the result, is it because of the 3D-printed model or something else?"
Many preliminary studies have reported there are potential benefits of integrating VR and 3D printing into medicine, he continued. "But is it really true that [VR and] 3D printing add clinical value? A lot of research is needed beyond some case reports about how fantastic the techniques are," he said.
For their part, Brouwers and colleagues are currently creating individually tailored 3D-printed prosthetics based on medical images acquired using a handheld 3D scanner for residents of Sierra Leone.