A detailed investigation of the CT head stroke pathway -- from when a scan request is made to generation of a final report -- has led to the creation of a 10-point plan of action to improve service delivery at a hospital group in northwest England.
Data for the St. Helens and Knowsley National Health Service (NHS) Trust in Merseyside, U.K., showed the combined average time from a patient's scan being ordered to reported was 59 minutes between September and November 2018. This is acceptable, but there is scope for improvement, particularly in terms of better liaison with the stroke team and more education and communication, according to Katie Sharkey and Katy Marsh, radiographers at the NHS Trust.
"Liaising and communicating with radiologists, especially out of hours, is crucial to ensure a timely report," they told delegates at the UK Imaging & Oncology Congress (UKIO) in Liverpool. "Education into accurate postprocessing is required, and reminding referrers to use the correct urgency code to filter head CT requests."
They proposed the following 10-point plan:
- A stroke bleep for members of the stroke team provides a direct way to contact CT radiographers if phone lines are busy.
- Radiographers should attend monthly scrutiny meetings with the stroke team to highlight areas for improvement.
- Reviewing images whilst the patient is on the scanner could indicate if any further scans (e.g., angiograms) need to be performed immediately. Also, encourage the administration of thrombolysis while the patient is on the scanner, Sharkey and Marsh recommended.
- Stroke patients should be prioritized by all staff groups, including porters, accident and emergency (A&E) staff, radiographers, and radiologists.
- Evidence shows there is a large variance in postprocessing. Radiographers must be reminded about the importance of accurate postprocessing.
- Educate radiographers about common appearances of pathologies on CT head scans that may contraindicate thrombolysis.
- Educate referrers about the code system for requests and the importance of using the correct code.
- Ensure radiologists are aware when thrombolysis patients are scanned, especially out of hours.
- Document any information relevant to the patient's pathway on the computerized RIS -- e.g., if the patient is too unwell to attend their scan or staffing issues.
- Ensure an efficient and effective handover at the end of every shift.
The national picture
More than 100,000 strokes a year occur in the U.K. alone, equating to a stroke about every five minutes, and strokes are now the fourth leading cause of death in the U.K., costing the economy about 26 billion pounds (29.4 billion euros) every year, Sharkey and Marsh reported.
The National Institute for Health and Care Excellence (NICE) state if a patient meets the guidelines, a nonenhanced CT scan of the head should be completed "immediately" -- defined as "ideally the next slot and definitely within one hour, whichever is sooner." Alteplase, the thrombolytic drug, should be administered within 4.5 hours of symptom onset. It is more effective the quicker it is administered, but, in some cases, it can be administered up to six hours after system onset, they explained.
The authors wanted to check if their NHS Trust met the NICE stroke guidelines and examine the effectiveness of their hospital group's pathway. They collected data from a CT scanner not based in the A&E department. Their inclusion criteria were any request using the computerized RIS "urgency 2 code." They excluded any requests with other codes.
The results are shown below.
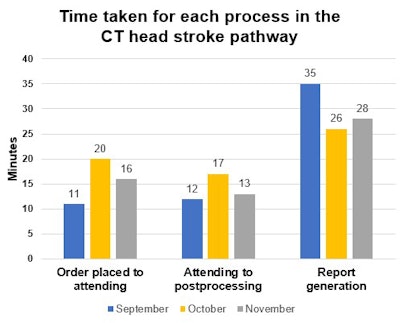
October had the largest delay in patients attending and postprocessing, but also the quickest average reporting time. The pathway for that month was slightly longer (63 minutes). September was quickest for attendances and postprocessing, but it also had the highest average delay for a report. November was marginally quicker overall, with completion of the pathway in an average of 57 minutes.
The authors found there was a slightly higher delay in reporting out of hours and across handover times in October, but they could not identify a reason for the inconsistencies.
Overall, the audit found the authors' hospital group is meeting the NICE guidelines. After making service improvements over the coming months, the group plans to carry out another audit to create a more representative sample. This second audit will serve to illustrate how the improvements have had an effect on the stroke pathway in accident and emergency, they noted.
"The invaluable relationship between stroke nurse specialists and radiographers should not be overlooked in providing a high-quality service," the authors stated. Experienced U.K. "Band 6 radiographers can accept CT head requests that meet the NICE guidelines within their scope of practice, contributing to the efficiency of the pathway."
A limitation of this audit is it excluded any stroke patients incorrectly entered under the wrong urgency code on the RIS. This may have limited the sample size, they concluded.