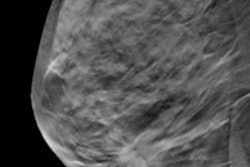
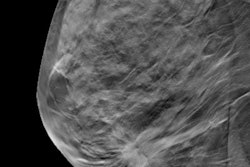
Swedish researchers have found digital breast tomosynthesis (DBT) and digital mammography seem to detect cancers of a similar biologic profile. Their findings were published online on 3 September by Radiology.
The results demonstrate that DBT screening doesn't "alter the predictive and prognostic profile of screening-detected cancers," wrote a team led by Dr. Kristin Johnson of Lund University.
 Dr. Kristin Johnson of Lund University.
Dr. Kristin Johnson of Lund University."The biologic profile of the additional cancers detected at digital breast tomosynthesis in a large prospective population-based screening trial was similar to those detected at digital mammography, and the majority were early-stage luminal A-like cancers," the group wrote.
DBT has the potential to become a widespread screening modality, according to Johnson and colleagues. But data regarding its performance for identifying tumor characteristics have been limited.
"So far, it has been shown that DBT (alone or in addition to digital mammography) depicts additional cancers, both invasive and in situ; the former is mainly early-stage hormone receptor-positive (i.e., luminal) cancers," the group wrote. "Because DBT is especially sensitive in the depiction of spiculated tumors, an imaging feature associated with favorable prognosis, we hypothesized that the additional cancers detected at DBT screening mainly would be of less aggressive subtypes."
Johnson and colleagues conducted their study to describe the tumor characteristics, including molecular subtypes, of additional cancers found on DBT compared to those found on digital mammography. They used data from the Malmö Breast Tomosynthesis Screening Trial, which included 14,848 women. Among these women, 139 cancers were identified: 118 were invasive and 21 were ductal carcinomas in situ (DCIS). Of the 139 cancers, 89 were identified by both digital mammography and DBT, 42 by DBT alone, and eight by digital mammography alone. Of the 118 invasive cancers, 37 were detected on DBT alone.
Johnson's team assessed breast cancer tumor characteristics and classified invasive cancers according to the following:
- Luminal A-like
- Luminal B-like human epidermal growth factor receptor 2 (HER2)-negative
- Luminal B-like HER2-positive
- Nonluminal HER2-positive
- Triple negative
The researchers found no statistically significant differences between DBT and digital mammography in the distribution of tumor size 20 mm or smaller, node-negative status, or luminal A-like subtype. DBT's performance by subtype for additional cancers was comparable to that of digital mammography.
| DBT vs. digital mammography by tumor subtype | ||
| Tumor subtype | Digital mammography | DBT |
| Luminal A-like | 46% | 51% |
| Luminal B-like HER2-negative | 43% | 35% |
| Luminal B-like HER2-positive | 1% | 0% |
| Nonluminal HER2-positive | 4% | 3% |
| Triple negative | 5% | 8% |
The study findings offer further support for the use of DBT as a breast cancer screening modality, according to Johnson and colleagues.
"Our results suggest that DBT screening will not necessarily change the panorama of biologic profiles of screen-detected cancers, but rather that more of the same type of cancers would be detected," they concluded.