Early detection of vascular complications of liver transplantation is vital to establish effective treatment, and this can determine the outcome of transplantation, patient mortality, and morbidity, according to an experienced group of gastrointestinal and abdominal imaging specialists from Valencia, Spain.
"Clinical manifestations of liver transplantation complications can be subtle and nonspecific. Medical imaging, mainly Doppler ultrasound, plays an important role to detect and grade these," stated radiologist Dr. Juan-José Delgado-Moraleda and colleagues at the Medical Imaging Department and Biomedical Imaging Research Group, La Fe Polytechnics, and University Hospital and Health Research Institute.
Color Doppler ultrasound exams are routinely performed at 24 to 48 hours on the seventh day, the first and third month after transplantation, while CT and MR images are acquired based on the Doppler ultrasound findings even in the absence of abnormal liver function, they explained in an in-depth article posted on 14 August by Insights into Imaging.
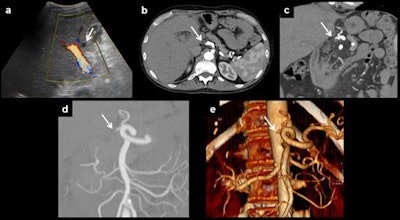 Anastomotic thrombosis. Artery thrombosis, the most serious complication of orthotopic liver transplantation, can be demonstrated as an absence of flow on Doppler ultrasound (a). CT can depict the thrombus and also the absence of distal flow (b). Multiplanar reconstructions and volume rendering images can be useful to ensure diagnosis (c-e). All images courtesy of Dr. Juan-José Delgado-Moraleda and Insights into Imaging.
Anastomotic thrombosis. Artery thrombosis, the most serious complication of orthotopic liver transplantation, can be demonstrated as an absence of flow on Doppler ultrasound (a). CT can depict the thrombus and also the absence of distal flow (b). Multiplanar reconstructions and volume rendering images can be useful to ensure diagnosis (c-e). All images courtesy of Dr. Juan-José Delgado-Moraleda and Insights into Imaging.The reported incidence of vascular complications is around 7% for cadaveric donor liver transplantation and around 13% for living donor liver transplantation, the authors wrote. Vascular abnormalities are associated with a high incidence of graft loss and mortality.
"As the clinical manifestations related to vascular injuries are nonspecific, early radiological examination plays a major role to make an early diagnosis and establish the best treatment options. Early endovascular treatment is correlated with liver transplantation salvage making early imaging studies especially important," they added.
 After treatment control. Control performed after thrombolysis and angioplasty of patient in previous figure. Normal arterial flow is seen. Resistive index shows normal values (0.6).
After treatment control. Control performed after thrombolysis and angioplasty of patient in previous figure. Normal arterial flow is seen. Resistive index shows normal values (0.6).Because vascular complications appear early after surgery, Doppler ultrasound should be performed by experienced staff; diagnostic angiography is seldom performed.
How they do it in Valencia
For vascular imaging evaluations, the following protocol is used at the facility in Valencia, where more than 100 cadaveric liver transplants are performed each year:
- Postoperative color Doppler must be performed after 24/48 hours and on day seven after surgery. Most patients also have a color Doppler at the first and third months.
- Contrast-enhanced CT is performed when a vascular lesion is observed on color Doppler images or when the liver function is impaired. Occasionally, MR is performed if contraindications to contrast-enhanced CT are present.
- T-tube cholangiography images with direct opacification are also performed on day four and the third month to assess the biliary tree.
- Hepatic intraoperative ultrasonography, which has emerged as a new technique, allows real-time evaluation of the anastomosis and immediate treatment before abdominal closure.
The main imaging findings in patients after liver transplantation are hepatic artery complications (such as thrombosis, stenosis of the anastomosis, and pseudoaneurysms), portal vein abnormalities (such as occlusion and stenosis), and hepatic veins and/or inferior vena cava flow changes (Budd-Chiari syndrome).
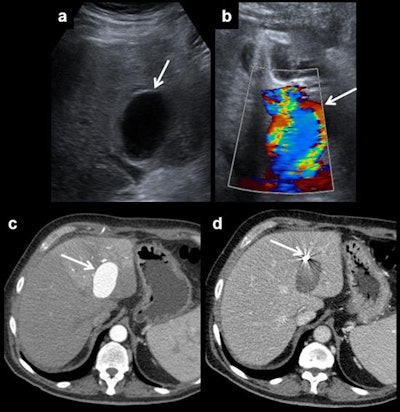 Hepatic artery pseudoaneurysm. Pseudoaneurysms can be discovered using ultrasound (a). It shows a characteristic appearance on Doppler ultrasound due to the turbulent forward and backward flow (b). Arterial phase CT shows arterial enhancement of the pseudoaneurysm (c). A coil is placed to block entry to the bloodstream and to prevent rupture (d).
Hepatic artery pseudoaneurysm. Pseudoaneurysms can be discovered using ultrasound (a). It shows a characteristic appearance on Doppler ultrasound due to the turbulent forward and backward flow (b). Arterial phase CT shows arterial enhancement of the pseudoaneurysm (c). A coil is placed to block entry to the bloodstream and to prevent rupture (d).Usual post-transplantation findings include right-sided pleural effusion, ascites, perihepatic hematoma, and periportal edema. All of them should resolve in the first weeks after surgery.
"Vascular and biliary anastomoses should be assessed by color Doppler," noted Delgado-Moraleda and co-authors Dr. Carmen Ballester-Vallés and Prof. Luis Marti-Bonmati. "Radiologists should have a clear knowledge of the individual patient postoperative anatomy because anastomoses are the locations where complications occur most frequently. Moreover, it is important to be aware of the anatomic variants, both in the donor and in the recipient."
The most common surgical technique is orthotopic liver transplantation where the graft is placed in the right upper quadrant, at the anatomical liver location, after removal of the native liver. Four anastomoses should be carefully assessed: portal vein, bile duct, anastomosis of the recipient inferior vena cava to the donor hepatic veins, and anastomosis of the hepatic artery.
The most frequently affected anastomosis is at the hepatic artery, they continued. This anastomosis can be made in different places, but the two most frequent are in the hair-pin space between the right and left hepatic arteries of the recipient or at the outlet of the gastroduodenal artery.
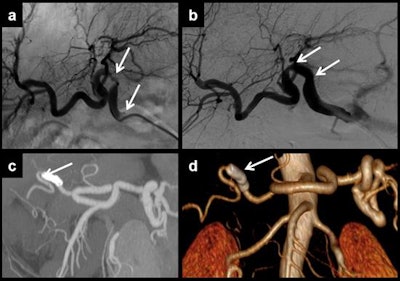 Multiplanar and 3D curved reformatting are useful to measure the vessel lumen in cases of multifocal stenosis of the hepatic artery. Each stenosis should be treated separately. In this case, angiography demonstrated two points of stenosis (a, b). Two stents were placed for treatment. Control CT showed that stents had been correctly placed. Distal artery flow is shown in the maximum intensity projection reconstruction (c) and in the volume-rendered reconstruction (d).
Multiplanar and 3D curved reformatting are useful to measure the vessel lumen in cases of multifocal stenosis of the hepatic artery. Each stenosis should be treated separately. In this case, angiography demonstrated two points of stenosis (a, b). Two stents were placed for treatment. Control CT showed that stents had been correctly placed. Distal artery flow is shown in the maximum intensity projection reconstruction (c) and in the volume-rendered reconstruction (d)."Stenosis may progress to thrombosis. So, stenosis and thrombosis are two entities of the same spectrum of vascular complications of liver transplantation," the authors wrote. "Stenosis can lead to splenic steal artery syndrome. It usually occurs in the first three months, but this time shows differences between patients, describing cases that happen even several years after surgery. Doppler ultrasound is the most useful technique to show this complication, as explained for thrombosis."
In the first three days after liver transplantation, an increased resistance index of the hepatic artery (greater than 0.8) is found in approximately 50% of the patients, they pointed out. If found, it should be monitored until it has normalized, typically on the fourth day after transplantation. Although the severity of the described findings correlates with the degree of the stenosis, ultrasound does not allow proper quantification of this, and the technique of choice is CT angiography. In addition, CT allows proper evaluation of patients with a poor sonographic window while MR angiography is a limited technique because of a relatively high false-positive rate, they added.
"Hepatic artery stenosis requires early treatment. First, an angiography and an angioplasty should be made. If this procedure fails, surgery is required. Once again, retransplantation has a better outcome, but is preferred as a second-line treatment to use when endovascular therapy does not work," they concluded.