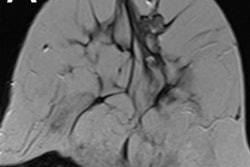
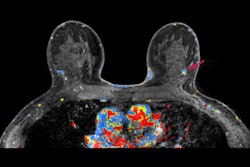
MRI finds breast cancer earlier than digital mammography in women with a family history of the disease but without known genetic mutations, according to research published online on 17 June in Lancet Oncology. But the improved detection comes at a risk of more false positives.
The study results could translate into better outcomes for this population of women, noted lead authors Dr. Sepideh Saadatmand and Amarens Geuzinge, of Erasmus University Medical Center in the Netherlands, and colleagues.
"MRI screening might lead to a substantial reduction in mortality compared with mammography screening," the authors wrote.
About 15% of all breast cancers arise in women with a family history of the disease but with no known hereditary gene mutation, and these women are at greater risk at a younger age, the group noted. Although previous studies have shown that adding breast MRI to mammography improves early breast cancer detection in this population of women, guidelines around the world are inconsistent.
Saadatmand, Geuzinge, and colleagues sought to remedy this by comparing MRI screening to mammography in women with familial risk of breast cancer in a multicenter randomized controlled trial called the Familial MRI Screening study (FaMRIsc).
The study included data from 1,355 women between the ages of 30 and 55 who had a cumulative lifetime breast cancer risk of at least 20% because of a family predisposition but who did not have BRCA1, BRCA2, or TP53 mutations. The women were recruited from 12 outpatient breast cancer clinics at seven academic medical centers and five hospitals. They were randomized into two groups: annual MRI and clinical breast exam plus biennial mammography (675), or annual mammography and clinical breast exam (680).
The study's primary outcomes were number, size, and nodal status of detected breast cancers. The study timeframe was January 2011 to December 2017, and the mean number of screening rounds per woman was four.
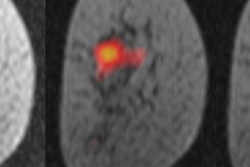
In the study cohort, 55 cancers were identified, 32 of which were invasive and 23 of which were ductal carcinoma in situ (DCIS). The team found that breast MRI had better primary outcomes than mammography.
| Breast MRI vs. screening mammography for breast cancer | ||
| Performance measure | Mammography group | Breast MRI group |
| Screen-detected cancers | 87% | 98% |
| Breast cancers identified per 1,000 screening rounds | 4.9 | 14.2 |
| Invasive screen-detected cancers per 1,000 screening rounds | 2 | 8.2 |
The researchers also found that invasive cancers were smaller in the MRI group than in the mammography group (median size, 9 mm versus 17 mm) and less frequently node positive (17% versus 63%). Tumor stages were also earlier in the MRI group compared with the mammography group (48% versus 7%).
"The number of cancers detected was significantly higher in the MRI group than in the mammography group. ... MRI screening resulted in lower numbers of late-stage cancers and node-positive cancers than mammography screening, thus both tumor stage and nodal status were significantly more favorable in the MRI group," the authors wrote.
Drawbacks to breast MRI, however, include the potential for more false positives. The study saw a high number of false positives, which the researchers attributed to the relatively young age of the study population.
The research shows that breast MRI is a powerful tool in a population of women at higher risk of cancer due to family history, according to the authors.
"We conclude that in real-life practice, MRI screening can result in an important and favorable shift in tumor stage at time of breast cancer detection compared with mammography screening, reducing the incidence of late-stage cancers and thus reducing the need for adjuvant chemotherapy and the risk of mortality," they concluded.