Danish researchers have found that fluoroethyl-tyrosine (FET)-PET can help confirm the success of surgical procedures performed on children with brain and spinal cord tumors to ensure that no residual tumor is left behind. Their study was published online on 25 January in the Journal of Nuclear Medicine.
Danish researchers found that FET-PET scans added "relevant clinical information" in 41% of cases by eliminating the need for immediate follow-up resection. In one case, it identified an additional tumor that MRI missed.
The information provided by FET-PET could, therefore, enable clinicians to follow patients more conservatively, rather than subjecting them to another surgery.
"If reoperation is considered based on an early postoperative MRI, our results support that additional F-18 FET-PET could help discriminating treatment effects from true residual tumor, allowing for a conservative approach instead of immediate reoperation for a number of children where F-18 FET-PET does not suggest residual tumor," wrote the researchers led by Dr. Lisbeth Marner from Copenhagen University Hospital Rigshospitalet.
When clinicians find pediatric brain tumors, complete resection is the most common course of action. While an early postoperative MRI scan can help determine the success of the surgical procedure, the results may be "misleading due to MRI signal changes caused by the operation," the researchers noted.
On the other hand, FET-PET has shown it can provide excellent accuracy for residual tumor detection, compared with MRI, among adults after surgery for glioblastoma. The key is the tracer's ability to differentiate between tumor and normal brain tissue.
There is limited information, however, on the use of FET-PET in pediatric patients for neuro-oncology cases. Thus, Marner and colleagues investigated the efficacy of postoperative FET-PET in children and adolescents after surgery for a brain or spinal cord tumor using simultaneous PET/MRI. They compared FET-PET's sensitivity, specificity, and accuracy for detecting residual tumors with the results of MRI alone.
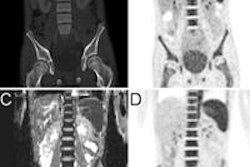
For this prospective study, the researchers consecutively enrolled 22 patients with a mean age of 9.5 years (range, 0-19 years) between March 2015 and October 2017. During that time, a total of 27 early postoperative FET-PET scans were performed on a PET/MRI (Biograph mMR, Siemens Healthineers) or PET/CT system (Biograph TruePoint, Siemens). The researchers then used follow-up (93%) or reoperation (7%) as their reference standard.
Marner and colleagues found that FET-PET added relevant clinical information in 11 of the 27 cases (41%); this included confirmation of a successful procedure and no need for immediate additional surgery. In one case, FET-PET detected an additional small lesion that was not seen on MRI. The discovery prompted a follow-up resection.
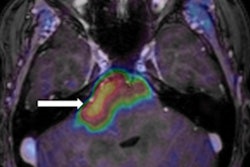
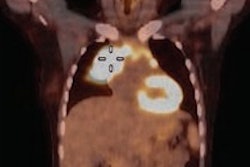
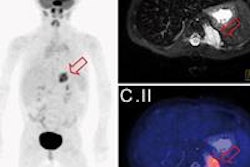
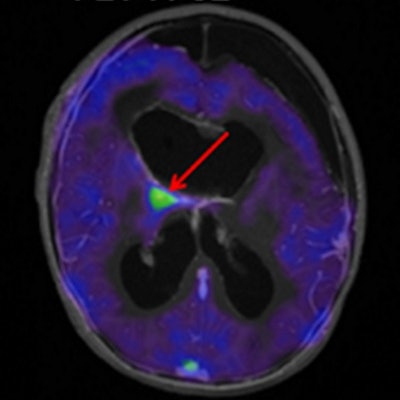
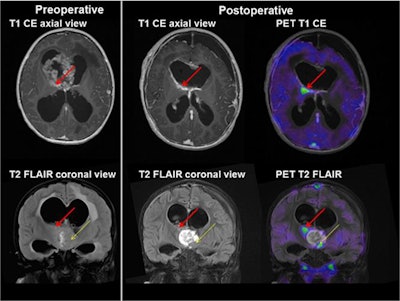 Axial (top) and coronal views (bottom) from 3-year-old boy with a grade IV atypical teratoid/rhabdoid tumor. A large intraventricular contrast-enhancing tumor mass (left column) was discovered preoperatively. Postoperative MRI identified a contrast-enhancing residual tumor inferiorly in the resection cavity (thin yellow arrow). An additional small residual tumor (red arrow) was identified only by FET-PET. Complete resection was obtained by removing both residual tumor masses. The patient received radiochemotherapy and is in long-term remission. Images courtesy of JNM.
Axial (top) and coronal views (bottom) from 3-year-old boy with a grade IV atypical teratoid/rhabdoid tumor. A large intraventricular contrast-enhancing tumor mass (left column) was discovered preoperatively. Postoperative MRI identified a contrast-enhancing residual tumor inferiorly in the resection cavity (thin yellow arrow). An additional small residual tumor (red arrow) was identified only by FET-PET. Complete resection was obtained by removing both residual tumor masses. The patient received radiochemotherapy and is in long-term remission. Images courtesy of JNM.Early postoperative FET-PET/MRI achieved lesion specificity of 100%, compared with 75% for MRI alone. FET-PET/MRI also had better accuracy (87%) than MRI alone (77%). Regarding sensitivity, MRI alone (80%) was superior to FET-PET/MRI (73%).
The results indicate that FET-PET/MRI can be a "powerful research tool that may help advance pediatric neuro-oncology in the future," Marner and colleagues concluded.