Ultrasound is 98% effective for further assessing masses found on screening digital breast tomosynthesis (DBT), according to a study published online on 29 November in the British Journal of Radiology. The findings suggest that a diagnostic mammogram after screening DBT is unnecessary, thus sparing women additional radiation exposure.
"There is potential for avoiding a diagnostic mammogram for evaluation of the majority of digital breast tomosynthesis screen-detected masses," wrote a team led by Dr. Sadia Choudhery of the Mayo Clinic in Rochester, MN.
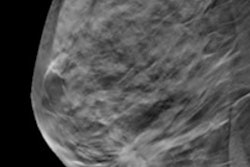
Traditionally, masses recalled on 2D screening mammography have been imaged with another mammography exam using specific diagnostic views before being sent to ultrasound, the group wrote. But compared with 2D mammography, screening DBT better visualizes lesions and boosts margin visibility, demonstrating similar accuracy with 2D for noncalcified findings, and comparable characterization of masses as benign or malignant.
This has prompted some breast imagers to suggest that diagnostic mammography may not be necessary after DBT.
"In the era of DBT, the need for diagnostic mammography before a diagnostic ultrasound for masses recalled from screening tomosynthesis has been questioned," Choudhery and colleagues noted.
Currently, wide variation exists among clinicians and institutions as to how to work up masses found on DBT, with some practitioners sending women directly to ultrasound and others to diagnostic mammography, then ultrasound, according to the researchers. They sought to explore whether diagnostic mammography is even necessary to evaluate masses found on DBT.
Choudhery's group conducted a study that included 212 masses recalled on screening DBT between July and December 2017 that were sent to either diagnostic mammography or ultrasound. The researchers tracked the size, shape, margins, visibility on ultrasound, diagnostic assessment, and pathology of all the masses, as well as each woman's breast density.
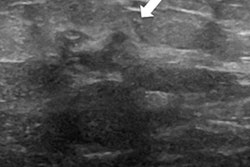
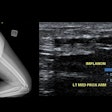
Of the 212 masses, 102 were worked up with diagnostic mammography and 110 with ultrasound. The group found no significant difference in the visibility of the masses sent to mammography first compared with those that were sent to ultrasound first or in the size of the masses or density of the women's breast tissue.
In fact, the study showed that 92% of masses sent to mammography first for follow-up were further evaluated with diagnostic ultrasound, and ultrasound successfully visualized 96% of those, the investigators noted. In addition, 98% of masses sent to ultrasound first were accurately assessed just with ultrasound.
"Our study indicates that the majority ... of masses ... recalled from screening DBT can be adequately assessed with a diagnostic ultrasound alone," the authors wrote. "This indicates a possibility to forego diagnostic mammography for workup of the majority of DBT screen-detected masses."
Cutting diagnostic mammography from the postscreening DBT process has a number of benefits, according to Choudhery's team.
"Eliminating diagnostic mammography can decrease cost and radiation to patients and increase diagnostic workflow efficiency for radiology practices," the group concluded.